Update From Modern Aging Singapore: Kickoff Workshop

Modern Aging Singapore kicked off in the middle of August. So far, the program has seen active participation and support from aspiring entrepreneurs. About three hundred students, health practitioners, researchers, and members of the public attended the Kickoff Workshop held at the NUS I Cube Building Auditorium on the morning of August 15.
Attendees were treated to four presentations from experts in aging and business: Overview of Aging by Prof. Angelique Chan of Duke-NUS Graduate Medical School, Healthcare and Business by Dr. Jeremy Lim of Oliver Wyman, Home and Center Based Care by Dr. Ng Wai Chong of the Tsao Foundation, and Product Design for Seniors by Hunn Wai of design firm Lanzavecchia + Wai.
 Prof. Chan highlighted some key trends and statistics on aging in Singapore. One surprising point was the high prevalence of social isolation among seniors here. This finding spurred aspiring entrepreneurs to think of novel solutions to address this trend.
Prof. Chan highlighted some key trends and statistics on aging in Singapore. One surprising point was the high prevalence of social isolation among seniors here. This finding spurred aspiring entrepreneurs to think of novel solutions to address this trend.
Dr. Lim went on to outline the aging sector in terms of business potential. One suprising finding, according to theNational Center for Policy Analysis, is the average net worth in 2010 was 848,000 USD for sixty five to seventy four year olds and nearly seven hundred thousand dollars for those above seventy five. These figures encouraged aspiring entrepreneurs to enter the aging sector.
Dr. Ng discussed the current status of home and center based care in Singapore. He highlighted specific needs in these care settings frequently used by seniors. This discussion allowed aspiring entrepreneurs to hone in on key areas of need and address these pain points. For example, some challenges in these settings include the quick and painless transferring of patients from bed to chair and vice versa, and increasing the time health practitioners can spend with seniors.
Mr. Wai rounded off the presentations with insights from product and design perspectives. He introduced examples of good design for seniors, such as mixed use canes and walkers, or stylish back braces. This presentation especially inspired aspiring entrepreneurs to consider seniors’ lifestyles and tastes when introducing new product ideas.
In addition to expert presentations, attendees also heard two senior role models share their life experiences and lessons. Younger members of the audience seemed glad to hear the wise advice dispensed by the seniors. The kickoff event concluded with a networking lunch. Participants became so engrossed in conversations around aging that they lingered past the scheduled end time.
Currently, Modern Aging Singapore has progressed to the business curriculum and selection phase. The top twenty teams have been selected and paired with industry mentors to hone their business ideas. The twenty teams will soon be pitching at the semifinals judging event for the top six spots. Meanwhile, all participants of Modern Aging Singapore are able to access the same business and aging curriculum on the Modern Aging Online Learning Portal to continue learning and improving their business ideas. If you would like to access the Portal, please write an email request to info@modernaging.org.
Find out more about Modern Aging, at www.modernaging.org.
TioHundra: How One Company Is Driving Innovation in Integrated Care
Mikael Thorberg, Sweden, has authored this blog post with Sofia Widén.
Our team at ACCESS Health International studies how countries deliver high quality and affordable elder care in Europe, Asia, and the United States. When we find promising and successful models, we analyze these models to understand their success. This blog post shares the results of one such study.
The healthcare sectors in many countries are innovating rapidly to meet the needs of aging populations. One of the most important opportunities in elder care is the development of new care models designed specifically to respond to the needs of an aging population. The elderly require care that is long term, integrated across multiple levels, and coordinated among different care providers. This care must be high quality, but it must also be affordable to the payers, be they individuals, insurance companies, or governments.
The ability to deliver on the promise of high quality, affordable elder care is no easy task, but many examples of promising models exist. In this blog post, we profile one such example: Care Company TioHundra, a public healthcare company in Sweden.
A Unique Model
TioHundra provides healthcare, homecare, and social care in Norrtälje, a city in Stockholm County. Throughout most of Sweden, counties oversee healthcare, and municipalities are responsible for providing homecare and social care. The two levels of government fund care separately and often do not communicate with one another, despite responsibility for the care of shared patients. At its formation, TioHundra took a unique approach to providing integrated care. Rather than attempting to coordinate care across multiple organizations and payers, TioHundra merged care providers and created its own payer. TioHundra now operates as one large healthcare and social care system, owned and managed jointly by the municipality and the county. This unusual merger represents one of the biggest regional reforms in Swedish healthcare in over twenty years. TioHundra is the largest employer in Norrtälje Municipality.
Information and Integration
TioHundra aims to integrate the entire care system in new and innovative ways. The objective of the company is to increase efficiency, quality, and safety while reducing the costs of care. As many as sixty people may be responsible for the care of a single elderly patient. Integration between hospitals and social care organizations enables TioHundra to overcome some of the friction and inefficiency that would inevitably result from large and uncoordinated care teams. One of the key benefits of integrated care is the relative ease with which information can flow between different care providers.
Healthcare providers use digital information systems to manage information about patients. Many counties and municipalities in Sweden use different digital information systems that are incompatible with each other. Likewise, a wide digital divide often exists between technologically advanced hospitals and traditional homecare organizations. The integrated structure of TioHundra enables different providers to access timely and accurate information about patients and their care plans. At this time, that information is in read only format. As a single, integrated provider, TioHundra is well positioned to introduce a single electronic health record system that allows different levels of access to different healthcare professionals. The company is exploring options to introduce such a unified system.
Technology alone will not improve the flow of information. Organizational integration is also vital to the seamless transfer of information. The leadership team at TioHundra works across organizational boundaries. A manager can pick up the phone, without hesitation, call another department manager, and immediately solve an issue. The focus at TioHundra is on patient care, not organizational boundaries. This focus on patient care is a crucial element of the integrated care model.
Payment and Incentives
A unified payment system is another key to the success of TioHundra and its integrated care model. Both Norrtälje Municipality and Stockholm County finance TioHundra, but the funds are channeled through a single entity. Elsewhere in Sweden, counties pay for healthcare through one avenue, while municipalities pay for homecare and social care through another. Payment through a single funder supports collaboration between healthcare providers and homecare and social care providers.
An integrated care system can also offer counties and municipalities the opportunity to explore payment models that reward positive health outcomes. The payment system should incentivize care providers to keep patients healthy. Dr. Peter Graf, Chief Operating Officer of TioHundra, recognizes this as an opportunity for improvement to the TioHundra integrated care model.
Many provider payment models encourage extensive care rather than positive patient outcomes. Currently, Stockholm County provides only sixty percent of reimbursements to providers based on capitation. Payments to providers based on capitation can encourage a focus on keeping patients healthy rather than delivering (and charging for) more care. The capitation rate of Stockholm County is the second lowest in Sweden.
It is relevant to question this model since, as Dr. Peter Graf puts it, “more care does not always result in better health outcomes”. An integrated care system is able to take a larger responsibility for patients, since it is a full service provider. An integrated care system along with the current technological development creates new opportunities to reward care organization based on health outcomes rather than on the number of services provided.
Challenges and Opportunities
The population of Norrtälje is aging even more rapidly than the population of Sweden overall. The lessons that Norrtälje Municipality and Stockholm County are learning through the innovations of TioHundra will provide valuable knowledge for anyone interested in the future of the Swedish healthcare system, elder care, and healthcare systems facing similar challenges.
Stockholm County and Norrtälje Municipality established TioHundra in 2006 as an experiment. The merger of healthcare, homecare, and social care at TioHundra is a complex process. The work of full integration is ongoing. Cultural differences across its component organizations add to the challenges of achieving full integration of care. TioHundra has had many successes, but the company is not without critics. Some areas of care have shown only limited progress toward full integration, and hospital readmission rates remain higher than desired. Until 2014, the company had been operating at a loss. Despite these challenges, TioHundra offers a living laboratory in which we can study the ongoing experiment in Norrtälje. The management team of TioHundra has shown a strong commitment to integrated care and sound financial management. The company broke even for the first time in 2014. We will keep an eye on TioHundra as the company continues to grow, continues to learn, and continues to improve how it provides integrated elder care.
Click here to download TioHundra Case Study: Part One.
Informal Child and Elder Care in Singapore: South Central Community Family Service Center
At ACCESS Health International, we like to feature good examples of community and elder care. A recent visit to the South Central Community Family Service Center in Singapore reveals a thriving space where different generations of neighbors visit, work, and play with one another.

The South Central Community Family Service Center is located in the southern part of Singapore. The Center is shown as a red dot on the map.
The South Central Community Family Service Center is just one of many other Family Service Centers in Singapore. Family Service Centers are an important part of the “Many Helping Hands” approach of the Singapore government toward social services. The Many Helping Hands approach emphasizes the involvement of multiple sectors in providing for the social welfare needs of people. Family Service Centers are run by Voluntary Welfare Organizations and are supported by the Ministry of Social and Family Development, the National Council of Social Services, Community Chest, or the Singapore Totalisator Board [1]. This is one way the government supports and encourages care provision by nongovernmental entities.
The South Central Community Family Service Center is unique in one respect. In January 2013, the Center became an independent entity with its own board of directors. The mission of South Central Community Family Service Center remains the same: to promote the wellbeing and self reliance of families. The main focus is supporting lower income individuals and families in the Bukit Ho Swee, Henderson, Redhill, and Indus Road neighborhoods. Between 2013 and 2014, the Center managed an average of four hundred cases. Casework involves counseling or referral to specialized services. For example, children from families lacking in basic necessities may face challenges in schoolwork or dealing with classmates. Center staff can counsel children or their parents on managing these problems. Where necessary, families are referred to other services, such as specialized psychiatric help or financial aid.
Besides casework, another focus of the Center is community engagement. To this end, Center staff organize events to involve nearby residents and create community spirit. As the Center is located on the ground floor of a block of residential flats, it is accessible and open to residents in the neighborhood. Our visit took place during the Lunar New Year period. As seen in the photo, festive decorations lining the entrance created a welcoming and friendly atmosphere.
Outreach worker Erwin showed us around the Center. Erwin explained to us that a guiding principle for the Center and staff is community cooperation and participation. This principle is informed by the Asset Based Community Development approach to community work. This approach ensures sustainability because initiatives are driven by the residents themselves. Residents volunteer to help care for their neighbors’ elderly relatives or children. Residents worked together to plant a community garden full of useful medicinal herbs.

Residents take ownership of the community garden and bond while caring for the plants. (Photo: South Central Community Family Service Center)
The Center is a collaborative environment. The community garden is a visible fruit of this collaborative environment. The garden had been an empty space in front of the Center. Center staff wanted to galvanize residents to work on a common project. Residents contributed ideas and voted for the winning project: a medicinal herb and vegetable garden. Because the idea came from residents, the garden has been adopted and cared for by residents.

Residents contribute ideas to keep the garden fresh and growing. Residents can vote for the next plant type by placing a marble in the respective bottle.
In the picture above, one can see a board where residents can vote on the next plant type. At the time of visit, sweet potato leaf was the leading candidate. The board itself was constructed by hand by a resident who is a carpenter by trade.
Inside the Center hangs another board, where residents can request items or services they need, or post offers of items or services they can give. The platform helps match community resources to people who need them most.
Residents streamed in and out of the Center throughout our visit. Erwin pointed out a pair of young siblings playing games on the couch. Erwin told me the siblings come to the Center after school ends to wait for their parents to get off work. I also saw groups of elderly chatting with one another at tables and chairs. The open space created by the South Central Community Family Service Center helps with informal child and elder care as residents look out for and engage with one another.
Near the end of our visit, there was a briefing for a large group of about twenty five volunteers, both young and old. They were preparing to give out yusheng packs to shop owners and residents at the Lengkok Bahru neighborhood. This showcased lower income families and children as goodwill ambassadors as part of this “Lo Hei Outreach”. The yusheng salad is traditionally eaten during the Lunar New Year, and Lo Hei is the dialect term for tossing the salad. Family and friends gather to Lo Hei together, signifying prosperity and togetherness. The briefing was punchy and positive with the staff recognizing the contributions of volunteers.
The South Central Community Family Service Center is an example of successful informal community and elder care. The staff and volunteers have created an open venue where residents are encouraged to join community activities and contribute their talents. Can their model of community involvement and ownership be replicated elsewhere? For example, could elder care as a larger industry move toward being more community based and operated? Share your thoughts with us by leaving a comment.
1. The Singapore Totalisator Board, also known as Tote Board, manages the surplus funds generated by Singapore Turf Club and Singapore Pools. They channel funds in support of various causes in Singapore such as arts and culture, social services, community development, education, health, and sports.
US House of Representatives Votes to Repeal Medicare Sustainable Growth Rate and Strengthen Medicare Access

The United States Capitol Building. (Photo: House Press Gallery)
We at ACCESS Health have been watching the news closely for the last two weeks. The issue of interest was the vote by the United States (US) House of Representatives on March 26 to repeal the Medicare sustainable growth rate formula and to “strengthen Medicare access by improving physician payments and making other improvements.” The bill can be viewed here.
This event is noteworthy in a few ways. One is that the 392 to 37 vote reveals overwhelming bipartisan support for these changes. Another is that, if passed by both houses of Congress, the bill would change the US healthcare payment system significantly. The bill still needs to be passed by the Senate.
If passed, how will the bill affect healthcare in the US? First, the bill repeals the sustainable growth rate formula used by Medicare. The sustainable growth rate formula pegs provider reimbursements to economic growth, as measured by gross domestic product (GDP). In place of the sustainable growth rate formula, the bill proposes value based payment models such as accountable care organizations and bundled payment. Accountable care organizations link doctors, hospitals, and other health professionals together to develop tailored care plans for Medicare patients. These care plans encompass the entire care process, matching the appropriate service to patients’ needs and reducing duplication of efforts. The bundled payment system reimburses care providers based on expected costs for specific clinical issues. This prevents unexpectedly high costs for patients.
Presently, the US healthcare system uses a fee for service model to pay providers. This means providers are paid for each individual service or operation, regardless of necessity or efficacy. As described in Forbes, “[Fee for service] actually rewards providers financially when patients suffer complications or infections, and pays them more if [providers] order unnecessary tests or procedures.”
Changing this system would remove incentives for healthcare providers to push large numbers of services on patients. Replacing fee for service with value based payment models could improve patient outcomes while reducing costs.
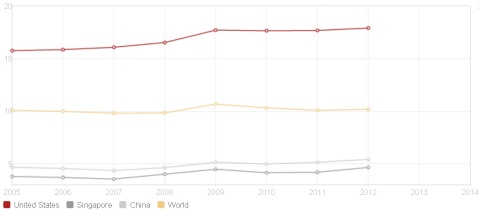
Spending on healthcare as a percentage of GDP in the United States, Singapore, and the world. (Picture: World Bank)
In the future, the high percentage of GDP spent on healthcare in the US may fall. According to World Bank data, the United States spent nearly eighteen percent of its GDP on healthcare in 2012, the highest in the world. GDP savings on healthcare would allow higher spending in other areas, such as education.
However, it is still too early to tell whether the bill will pass the Senate. In addition, there are still many challenges to the change. Many healthcare providers still cling to fees for services models of payment. It is also challenging to define key performance values for providers. Will providers aim to reduce readmission rates or improve life expectancies of patients? At this point, performance values are not standardized. Nevertheless, the strong bipartisan support for the bill shows a consensus that the existing sustainable growth rate model is undesirable.
This movement represents a move toward a capitation payment system, which pays providers a set amount for each patient, regardless of service type. Capitation systems are used by countries like Italy, the United Kingdom, and Denmark. In addition to the US, fee for service is used in countries like Japan, Germany, and Canada.
Interestingly, China has used the fee for service system since the 1980s. China has experienced healthcare cost increases, poor quality, and a questioning of medical ethics. These factors have led to experimental healthcare reforms, since the 2000s. City and local governments were encouraged by the central government to redesign the healthcare system, with wellbeing of patients as a main goal. China tried bundled payment systems, with some success. Jining saw a thirty three percent reduction in expenditure, while Shanghai saw a seven to twelve percent reduction in cost per outpatient visit. However, these initial results are not conclusive of the superiority of a capitation system. China continues to experiment with and review healthcare reforms.
If the US moves forward with the repeal of the sustained growth rate for Medicare, other countries facing challenges with fee for service healthcare models may follow suit. The ripples of this bill are potentially larger than domestic US healthcare policy. What do you think of these policy developments? Tell us your thoughts by leaving a comment.
Taking a Cue from Lee Kuan Yew on Aging Well

Mr. Lee celebrating his seventy seventh birthday with his wife, Kwa Geok Choo, on September 16, 2000. (Photo: Edward Wray, Associated Press)
Lee Kuan Yew, the founding prime minister of Singapore, passed away on Monday morning. As the first prime minister, Mr. Lee helped shape many policies in the formative years of independence. As the Singapore population matured, aging became an issue of concern for Mr. Lee. He shared some personal views on aging at a forum in 2010, when he himself was close to ninety.
Mr. Lee said, “I think the most important single lesson I learned in life was that if you isolate yourself, you’re done for. The human being is a social animal – he needs stimuli, he needs to meet people, to catch up with the world.”
Mr. Lee also said, “You must have an interest in life… If you’re not interested in the world and the world is not interested in you, the biggest punishment a man can receive is total isolation in a dungeon, black and complete withdrawal of all stimuli, that’s real torture.”
Indeed, part of aging well is maintaining social support and engagement in activities. Population trends in Singapore indicate that, in the future, many more elderly will be single and living alone. We must create opportunities to help these elderly avoid isolation.
How can this be done? Many are thinking of solutions. The ACCESS Health Singapore team spoke to a professor in architecture. She explained to us that simply adding a small space to common corridors for residents to sit and mingle can draw them out of their flats. Eventually, she said, the residents may venture down their blocks and into the community.
There must be other ways to help our elderly age well. People from all sectors are thinking of novel ways to make a difference in the Singapore silver industry, a promising development. Mr. Lee’s advice was for individuals to take an interest in the world and to avoid isolation. How we can help is to think of creative ways to encourage these individuals to do so.
Perhaps then we can live out Mr. Lee’s wish, “Have a purpose driven life and finish well, my friends.”
Technology and Aging: Read the Interview and Learn what the Elderly Want!
ACCESS Health studies good examples of elder care in Sweden. In a series of group interviews, the Swedish team of ACCESS Health meets with a group of senior citizens to understand their needs. In this interview, the participants discuss technology, share their views on Swedish healthcare, and tell us about their experiences as informal caregivers. When they learned about the work of ACCESS Health, the participants volunteered for the focus group. The focus group participants live in the city of Eskilstuna, one hour southwest of Stockholm.
The blog post of this week is an extract from a group interview conducted on December 31, 2014 with Gudrun Bergström, eighty six, Gujje Byström, eighty nine, Inga Brehmer, eighty eight, and Ingrid Svahn, eighty five.
This is an insightful and fun read! Enjoy!

Participants of the ACCESS Health technology focus group. From the left: Inga Brehmer, Gudrun Bergström, Ingrid Svahn, and Gujje Byström.
Interview
Inga Bremer (IB): My name is Inga Bremer. I am eighty eight years old. I am interested in technology. I own an iPad. I own a Doro telephone. [Doro is a company that developed a simplified mobile telephone for older users.] My Doro is easy to use. My Doro telephone is not a smartphone. Dora does develop smartphones for older consumers right now. I also own a laptop. I own other technical devices at home, such as a dishwasher and a washing machine. I also have a small automatic vacuum cleaner so that I do not need to vacuum constantly. I have three large flat screen televisions with over fifty channels. I would call myself mildly interested in technology.

Inga Brehmer shows her Doro telephone and her tablet, which she uses to listen to the radio, to view emails, and to take pictures.
Gudrun Bergström (GB): My name is Gudrun Bergström. I am eighty six years old. I love technology. I am handicapped. I have poor eyesight. Technical solutions help me live with my sight impairment. I do not own a smartphone. I own a Doro telephone.
I have one of the newest stationary computers that you can buy. I use a magnifying software program that helps me increase the size of the text of the documents on my computer. I own an external hardware product. This hardware product helps me to magnify texts and images so that I can read and see the images better. This program is called Zoom Text.
I wear a watch that reads the time for me out loud. That is a great device. I have hearing aids. I also have three televisions. I use my three televisions. I have connected my television in the kitchen with an external hard drive so that I can record programs and store them.
Sofia Widen (SW): Do you record a lot of television programs?
GB: Yes. It allows me to watch them when I want to watch the programs. It took some time to figure out how to record programs. Learning is a gradual process.
I buy technology products. The booklet with instructions is written in a small text. This is problematic. It is difficult for older consumers to read small text. I can read instructions with my magnifying program. My dream is that doctors will find a way to operate a new sight nerve into my eyes so that I regain my sight. We are not there yet.
SW: Do you use your computer to browse websites?
GB: I browse a lot of different websites. I disapprove of some things that people write on Facebook.
SW: Do you have a Facebook account?
GB: Of course. I am on Facebook.
SW: Are you active on other social media sites?
GB: No. I am not interested in blogging or in tweeting. I use Skype. I Skype with my family. I have a wireless internet connection in my apartment.
IB: We should have spoken before you, Gudrun. You have so many devices.
GB: I love technology. My husband was not interested in technology. I installed devices at home. I learn about new products. I want to buy them. More people my age ought to take an interest in technology. Technology can help the elderly.
Ingrid Svahn (IS): Technology is in your nature. Either, you understand technology or you do not.
GB: I disagree. Look at the young who adopt technology. Are they born with an ability to absorb technology quickly? I do not think so. The young set aside time to learn how to use the technology.
IS: My name is Ingrid Svahn. I just turned eighty five. My husband knew everything about technology. I never needed to learn. My husband passed away a few years ago. I use modern technology. I am not interested in technology. I had a computer. I threw it out when it crashed.
SW: What did you use your computer for?
IS: I served on the board of an organization. I used my computer to type out the minutes from our board meetings. I have a smartphone. I use my smartphone sometimes.
SW: How do use your smartphone?
IS: I play games. I like Alphabet and Scrabble. I will say, though, that like other retirees, I do not have time to play all these games. Many retired people I know say they are busy. I also feel that I am busy all the time. I also own televisions. I use a dishwasher and a vacuum cleaner.
I use a pen for my touchscreen smartphone. I do not have Wi-Fi. I access the internet through the mobile network. Other family members discuss what kind of technology I need. They discuss whether I should install Wi-Fi or not. I do not know how the discussion will end. I might buy a tablet.

From the left, Inga Brehmer with her Doro telephone and her tablet. In the middle, Gudrun Bergström, with her Doro telephone and her tablet. To the right, Ingrid Svahn with her smartphone.
GB: I recommend a tablet. Tablets are great. You can carry it around. You can carry a mobile phone of course. I would not compare the two products. A tablet is helpful for my reduced sight. I prefer a larger tablet.
Gujje Byström (GBO): I am eighty nine years old. I am not interested in technology. I own one television. I watch eleven channels. I dislike watching television during the day. I record my programs. I watch them in the evening.
From the left, Inga Brehmer with her Doro telephone and her tablet. In the middle, Gudrun Bergström, with her Doro telephone and her tablet. To the right, Ingrid Svahn with her smartphone.
GBO: I use hearing aids. I use a walker. The walker helps me when I shop. I can carry a lot of bags. I hang them on my walker. People pestered me to get a walker. I think it is wise to wait until you really need a walker before getting one. You become dependent on your walker. I could not manage to carry my groceries without my walker.
I prefer to use a cane. I have a beautiful cane. I like my cane. I have had hip and knee surgery. After my surgery I decided to get a cane. There are flowers on my cane.
IB: I have a cane. My doctor prescribed the cane, so I obtained it for free. We buy technology such as canes and walkers. We buy them because we want nicer versions. In Sweden, you obtain technical aids from your doctor or from your municipal care organization. The devices are almost free or charge. You pay up to a fixed sum every year. This is a low sum. If you pay the fixed sum, you can obtain all devices that you need.
GB: We can discuss if you always obtain all the devices and all the aids that you need. I have a friend who requested two walkers. She was refused those two walkers. She wanted one robust walker for outside use in the snow. She wanted a smaller walker for use inside her apartment.
I returned the walker I was given for free. I bought my own walker. Look at my walker. I can lift it. It is light. [Gudrun demonstrates. She brings out her walker to the focus group.]
GBO: Those walkers are expensive. You made an investment.
GB: I can carry up to seven bottles of wine with this walker!
SW: Can you use the walker with thin wheels outside in the snow?
GB: If it is that snowy I do not go outside. There is no reason for me to leave the house when I cannot walk on the streets. Most Swedish cities are not accessible to the elderly in the winter. Too much snow and ice on the pavement prevents the elderly from leaving their houses.
Södermanland County Council hands out two types of walkers: one with large wheels and one with smaller wheels. Rules vary from county to county because regional governments are autonomous. The number of aids that you can obtain from each county varies.
GBO: The design of certain walkers can hurt your shoulders. I experience pain in my shoulders because of the way I walk and what I carry. I never experienced pain in my shoulders before. I have experienced pain in all other parts of my body before. I never suffered pain in my shoulders before.
You will soon be able to read the entire interview, posted on the ACCESS Health website here.
TioHundra – A New Integrated Care Model for Sweden?
This blog post introduces Care Company TioHundra in Norrtälje, Sweden. This is a unique model of integrated care in Europe. I have had the opportunity to interview Peter Graf, Chief Operating Officer of TioHundra. Peter Graf talks openly about the challenges and the many opportunities that TioHundra faces. I have also had the opportunity to interview members of the staff and managers throughout the organization. Through these interviews, I have gained an understanding of the different parts of the company. I will tell you about my impressions of TioHundra in a series of blog posts. You can access the full interviews and all relevant background information from this case study on the ACCESS Health website.
Background
An older person with multiple diseases often requires care from several healthcare and care providers. This elderly patient may travel to a local hospital for treatment. It is not uncommon that up to sixty people from various care organizations are involved in the care of an older individual with complex care needs. Patients with complex care needs require the services of both the county healthcare providers and the local municipal care organizations. As individuals in Sweden age, and as more people live with multiple diseases and have complex care needs, counties and municipalities realize the need for greater care coordination. Care coordination to meet the needs of the elderly is one of the greatest challenges in Swedish healthcare, witnessed by the large effort of the previous center right coalition government to improve care coordination in the program “The Most Ill Elderly” from 2010 to 2014.[1] The previous government allocated over four billion Swedish kronor to improve the coordination of care for the most ill elderly. TioHundra shows that their model of integrated care already works well. During the program The Most Ill Elderly, TioHundra received funding based on the results they displayed in their work for the most elderly ill. These results included a reduction in unsuitable medication for the elderly and shorter wait times in the emergency room, among other areas.
Elsewhere in Sweden, regional governments manage the healthcare provision while local governments provide homecare and social care. Well defined areas of responsibility ensure that each provider in healthcare and in social care can focus on a range of services. In theory, the specialization of each level of government ensures that citizens obtain the healthcare and homecare they need. In practice, the division of responsibilities causes delays in service delivery, and at times, it compromises the quality of care. Regional and local governments use different communications systems, have distinctive work cultures, and use individual terminologies. Older frail patients, among other groups, suffer when healthcare providers fail to communicate effectively across organizations. TioHundra overcomes many problems of care coordination. Instead of coordinating care across organizations, TioHundra merged multiple care providers, now operating as one large healthcare and care system. This merger entails one of the largest regional reforms of Swedish healthcare since the Nobel Reform in 1992.
Care Company TioHundra is a public healthcare company that provides integrated care in Norrtälje, a city one hour north of Stockholm in Sweden. TioHundra operates an emergency hospital, six primary healthcare clinics, and a home healthcare organization for patients who are unable to travel to obtain care. It also manages social care and homecare organizations. The company runs nine nursing homes and it has 3,500 employees, including healthcare professionals and administrative staff.
To improve the quality of healthcare and to overcome the care coordination problems of regional and local administrations, Norrtälje and the Stockholm County Council established TioHundra in 2006.
Philosophy
The guiding philosophy of TioHundra is to construct an integrated healthcare system. The objective is to be the leader in integrated care in Sweden, and to be the number one choice of care provider in Norrtälje. The management approach centers on constant improvements. Managers and employees at all levels of the company identify areas for improvement, suggest new routines, and implement changes. The idea is to constantly improve service delivery and employee satisfaction.
Improved Care, Lower Cost
The ability to turn around negative operating results of previous years into a positive net result helped to convince politicians in the region that TioHundra improves the quality of care while lowering the delivery costs. Results from the employee survey show that the company employs a more satisfied workforce in 2014 than in 2013.
TioHundra manages to overcome certain problems of care coordination that persist in other regions and in other municipalities. Formal and informal channels of communication improve the transfer of information between different departments. Patient data is shared throughout the organization with the help of read only functions in patient journals. Weekly meetings of the management team foster an atmosphere of cooperation. Where disagreement occurs, the meetings serve as an arena for constructive debate.
Financing
TioHundra obtains one pool of financial resources from municipal and county taxes. Elsewhere, counties raise taxes for healthcare while municipalities raise separate taxes for social care. Budget silos prevent counties and municipalities to coordinate care in other parts of Sweden. One level of government is sometimes reluctant to deliver a service it considers to be the responsibility of the other level of government. The organizational structure of TioHundra allows this problem to be overcome through a lateral integration of caregivers from the county and the municipality.
Conclusion
In summary, TioHundra is a unique healthcare company. There are no other companies like TioHundra in Sweden. Few similar care organizations exist elsewhere in the Nordic countries. TioHundra reported a balanced budge for the first time in 2014. It also marked a year where management recorded improvements in employee satisfaction. TioHundra delivers healthcare of high quality at relatively low costs. The company has reduced the number of medications per older patient, reduced the prescription of unsuitable medications for the elderly, and it has shortened emergency room wait times for this patient group.
It remains to be seen how the integrated care model of TioHundra evolves. A transition in 2015 away from a focus on balancing the budget, towards operational and organizational changes is already noticeable. This is a young company with an eager management team. If the quality of care improves dramatically, and if the costs of healthcare can be contained in Norrtälje, other counties and municipalities may look into adopting the model of TioHundra.
[1] De mest sjuka äldre
New Tech for Old Age: A Growing Number of High Tech Solutions Aim to Improve Life for the Elderly
I spent two days participating in a conference in Stockholm on the topic of welfare technology.[1] Welfare technology is a term that encompasses a wide range of information and communications technologies, alarms, aids, devices in the home, and other technologies that help the elderly or people with disabilities. The official definition states,
“Welfare technology is the knowledge and the use of technologies that can contribute to increased safety, activity, participation, and independence for people with disabilities and their families. Welfare technology can also support independent living, and it can prevent or supplement healthcare and social care needs. Welfare technology can help to improve resource utilization and quality in the welfare sector, and it can be economically viable.”[2]
This conference was the first in Stockholm on the theme of welfare technology. I hope it will become a permanent and annual event.
The conference featured panel debates, lectures, and a round table discussion. Companies showcased their latest products. Economists lectured on the economics of technology in healthcare and social care. Lawyers described the legal framework and the regulation of technology. Participants exchanged ideas and networked.
As a researcher for ACCESS Health, I immersed myself in the latest thinking on welfare technology. I examined how the fusion of a bicycle, a computer game, and a chair can improve the health of the elderly. Read about the company that has developed this bicycle that allows a biker with poor balance to cycle in a three dimensional environment of his or her choosing.

A seated bike with display encourages exercise among the elderly. The sturdy seat ensures that no one falls off the bike. The curved screen tricks the rider’s mind into believing that she is riding her bike outside.
The idea of the bike is to stimulate more exercise. Equipment like this can turn exercise into an enjoyable experience for those who have suffered injuries and face months of painful rehabilitation. It can also encourage exercise in those who feel uncomfortable at a normal gym. Several municipalities in Sweden purchase the bikes, and the spinoff product, a treadmill that comes with a rounded screen to create the illusion of outside walking. This treadmill takes the person into a three dimensional reality. It works like a game. When the person looks to the left, the picture moves to the left. The user experiences a simulation of taking a stroll outside. The images are developed with Google street view. The tablet on the treadmill allows the user to play a quiz game while strolling in the forest. The questions are viewed on the large curved screen. The answers are recorded on the tablet. Developers believe that the gamification of exercise can enhance the user experience for the elderly.
The municipalities allow elderly citizens to come to community centers and to keep physically active. Perhaps we are witnessing the infancy of gyms with equipment developed for people over the age of seventy. This age group can benefit from exercise that strengthens muscles and trains the heart. Most public gyms do a poor job of installing exercise equipment and designing facilities that suit the needs of the elderly. I have been pleased to observe that developments in this area already benefit active older citizens.
I looked at the newest products on the market for safety alarm watches for patients who suffer from dementia, such as watches with positioning systems and alarms. I examined intelligent beds, which hold sensors in the mattress. The sensors notify caregiver personnel or are connected to your computer at home. The sensors highlight where there is pressure in the bed so that a caregiver can make adjustments and help the user avoid ulcers, which are a common result of pressure and poor blood circulation in certain areas of the body. The economists who participated in the conference, including Dr. Åke Dahlberg, calculate that these sorts of devices are so cost effective that the payer or user breaks even within one year of use. These calculations factor in the costs of treating an ulcer, which may demand that a patient visit a hospital twice a week.
The intelligent bed is an innovation produced at the Health Technology Center in Halland, in the south of Sweden. The bed is just one of many new technologies in the field of homecare and elder care that shows how patients can use smart technologies at home to prevent diseases and ulcers. These images display what nursing homes of the future may look like. The sensor, which goes under the mattress, can record your breathing and your pattern of sleep. To the right, a computer screen is visible. Doctors can use the data remotely to check up on you in the middle of the night and decide if you may need assistance at home.

This intelligent bed is an innovation of the Health Technology Center in Halland. The bed monitors sleep patterns, heart rate, and pulse.
You can read more about welfare technology in my upcoming case studies on the ACCESS Health website. I will shed light on the legal aspects of the use of technology in elder care. I will also examine the ethical aspects and discuss the economics behind the introduction of more technology in sectors like homecare, which largely center on personal meetings between caregivers and patients. This is an exciting area of development and shows promising results already. Patients, caregivers, and society at large stand to benefit from the technological advances in this sector. On the other hand, these technologies must be developed with the users in mind. The users are the healthcare staff, the homecare personnel, and the patients. A careful examination of patient needs and user friendliness for all of these groups must precede any introduction of technology in elder care and homecare. Far too many applications are developed without the involvement of the relevant consumers.
Previous waves of technology in these sectors illustrate that technology is powerful, and it will find users and needs for its applications. Previous waves of technology show that, in some areas, technology comes first and needs of the users come second. Developers apply technology from other fields to the elder care sector. This technology may not always be aligned with the needs of the users. The needs of the users must be the point of departure. Ideally, technology is not adopted from other fields; it is purposely constructed for older consumers, for caregivers, and for relatives. This is why the debate around technology is so important. The lecturers at the welfare technology conference stressed that they wanted to see technology that aligns with the needs of the users.
The previous generation of safety alarms for older people illustrates the point that technology does not meet the needs of users. The previous generation of safety alarms was connected to landline telephones. These alarms were a great invention for those who needed help at home. An older person who fell at home could use the alarm to contact a caregiver. The caregiver could come to the house and assist the person after the fall. However, the safety alarm could not be used on the balcony or outside of the house or apartment because it relied on the landline telephone. Sweden is introducing digital safety alarms on a large scale right now. The introduction has caused difficulties in many parts of the country, including disruptions in the signals to homecare personnel. Despite these difficulties, many municipalities are examining new digital alarms. In this process, some municipalities are introducing digital alarms that cannot be brought outside. The use of these types of alarms is a mistake. They confine the elderly to their apartments instead of encouraging an active lifestyle, which requires leaving the house.
Some new safety alarms, which often come in the form of watches to wear on the wrist, have Global Positioning System (GPS) technology built in, which allows a caregiver to turn on the navigation in his or her phone and navigate to the users, wherever he or she may be. The user can also talk into the watch and reach a caregiver, just like you would talk with someone on a mobile telephone. The image below illustrates a safety alarm with a positioning system and a clip on battery charger to ensure that the user does not lose the alarm when he or she charges the battery. Older versions of these watches must be taken off to be charged. A person with a cognitive impairment might easily forget to put the watch back on. Of course, the user must accept that he is traced when he wears the watch with a positioning system.
The new technology raises issues of privacy, data storage security, and surveillance of our elderly loved ones. Are we reducing or increasing their freedom with these alarms? As with any technology in the elder care sector, we must look at alternative solutions. No technology is perfect. Some technologies improve quality of life. If a technology has the potential to improve quality of life, we ought to examine the technology carefully.
In the case of wearable alarms with positioning systems, we either prohibit our loved ones from leaving the house alone because we are afraid that our elderly who suffer from dementia will become disoriented and wander off, or we allow these people to leave the house with a portable and traceable alarm system. Some people will be inherently skeptical of these technologies, perhaps more so in the wake of national programs on mass surveillance. There are arguments on both sides of this debate that need to be examined further, but the technologies show great potential.

The black safety alarm to the left is seen here on its charger. This type of alarm can be placed inside a pocket. The charger is developed for older patients to make charging easier. Patient put the alarm on the charger overnight. There is no need to plug in a small charger. This innovation greatly simplified the user experience for patients with Parkinson and similar conditions that affect motor skills.

The black safety alarm to the left is seen here on its charger. This type of alarm can be placed inside a pocket. The charger is developed for older patients to make charging easier. Patient put the alarm on the charger overnight. There is no need to plug in a small charger. This innovation greatly simplified the user experience for patients with Parkinson and similar conditions that affect motor skills.
The other ethical aspect we must think about carefully is consent. How do we obtain consent from users with cognitive disabilities? Is consent from relatives enough to allow the use of a safety alarm outside? It is impossible to offer one answer for all users and for all relatives. We must develop national guidelines that caregivers can follow. At each developmental stage, we must allow public lawyers to evaluate the legal implications of each technology. This will take time. We must be patient.
We must also allow individual caregivers and family members to decide what is best for their loved ones. What works for one user may be completely inappropriate for another user. Perhaps the user is bothered by a large safety alarm watch, scratching to take it off. In this case, I would think it wise to find other solutions. The elderly, like all of us, have different preferences. Common sense in the use of technologies will allow us to incorporate technology into sectors such as elder care and homecare. At the conference for welfare technology, nurses, lawyers, developers, and other participants raised these issues for debate.
Telia Healthcare, one of the largest telecom companies in Sweden, brought four showrooms to the technology fair in Stockholm. The product range HomeCare includes sensors in your bed. This bed is equipped with sensors in a pad that goes underneath the mattress. The pad warns if the patient lies still for too long or needs assistance to rise up. This pad is intended for use in care homes to guide the staff to the patient when the patient needs assistance. The blood pressure device on the bedside table can measure blood pressure and blood oxygen saturation. This information can be linked to patient records.
The sensors send signals via the Telia Healthcare application to caregivers or to the user. It is up to family members or users to decide where the text messages go. The bed below is equipped with a lamp gradually adapts to your sleeping pattern. It turns on a light in the morning to help you wake up. In cold, dark countries like Sweden, this may be a welcome device, although its healthcare application seems limited.

This bed is equipped with sensors in the white pad. The pad warns if the patient lies still for too long or needs assistance to rise up.

The small white sensor on the top left warns if a patient leaves the house. If the door opens, the sensor sends a text message to a caregiver.
A smart sensor at the front door of a person’s house can notify a caregiver if the user leaves his or her house and wanders off. The text message alert, combined with a traceable and wearable alarm, like the safety alarm watches discussed above, helps the caregiver to locate a person that may have gotten lost. Technologies like this could help an aging population to live at home for longer. They can also improve the sense of well being and safety for users and for family members. Telia intends to sell these products to public caregiver organizations in the spring of 2015. Municipal organizations develop new guidelines on public procurement, which includes data encryption for this type of product.
The small white sensor in the top left corner of the medical cabinet will send a notification if the cabinet has not been opened for a certain amount of time. The scales in the images below send weight information to your computer or to your caregivers, via Bluetooth. Fluctuations in weight are an early sign of declining health in patients suffering from chronic obstructive pulmonary disease, for example. The text message alert will act as a reminder for you to take your medication or visit your doctor before you develop more serious symptoms. All of these technologies will help patients with chronic diseases to live at home for longer in the future. The scales for home use stores information on patient weight. The scales can notify caregivers if a patient collects additional fluids, which is an indicator of rising blood pressure. The scales send the information via Bluetooth to the caregiver’s mobile telephone.
Now, Telia is just one of many companies entering the growing market of homecare devices. It remains to be seen whether these specific products serve the needs of these patients, or whether Telia must improve or change their products. Telia runs pilot studies with several Swedish municipalities where they evaluate their products.

The small white sensor on the top left signals to a caregiver if the patient forgets his or her medication at home. When the medicine cabinet opens, the alarm turns off.

This scale stores information on patient weight. The scales can notify caregivers if a patient collects additional fluids, which is an indicator of rising blood pressure. The scales send the information via Bluetooth to a mobile telephone.
Telia installs cameras for use at home during the night, when someone might otherwise need to visit the person to check that everything is in order. Several municipalities in Sweden work with eHomecare. eHomecare uses a camera that is switched on for a few minutes at a time throughout the night to check that the user is alright. This type of technology replaces short visits by homecare personnel in the middle of the night, and several users prefer a camera to personal visits. My upcoming interviews with the managers of eHomecare in Västerås stad will be posted on the ACCESS Health website.
In summary, the welfare technology conference stimulated important debates on technology for the elderly. I will keep you up to date on this important topic in future blog posts and in my case studies. I hope to see technologies that benefit the elderly. I want to see more companies that involve all users early on in product development. As one participant in the conference put it, “only when all groups benefit from the technology, including the doctors, the patients, the caregivers, and the relatives, can we expect large scale adoption.” One final reflection comes to mind the day after the technology conference. Many municipalities had representatives at the conference. Few county councils were present. If counties and municipalities want to stay up to date on the latest technology, this conference is a good starting point!
Too Good to Be True?
In my previous blog post, I described the work of the Mobile Team for the Elderly in Uppsala, Sweden, a municipality of two hundred thousand. In this blog post, I will discuss some of the tangible benefits of the Mobile Team to the municipality, to patients, and to patients’ families.
Before I get started, I want to explain how healthcare and government is managed and financed in Sweden. Sweden is organized into municipalities. Several municipalities comprise each county. Uppsala County includes eight municipalities, including a municipality called Uppsala municipality (see the maps below). Uppsala County manages healthcare provision for all citizens in the county. The County Council in Uppsala is the payer of healthcare in the county. An autonomous government governs each Swedish municipality. Municipalities are responsible for social care for the elderly. The Mobile Service offers healthcare to the elderly, thus touching on the responsibility of both Uppsala municipality and Uppsala County. The Mobile Emergency Team serves the elderly only in Uppsala municipality, not the entire county.

Uppsala County is located to the northwest of Stockholm County and to the east of Västmanland County

Uppsala Municipality borders the Municipalities of Östhammar, Tierp, Heby, Enköping, Håbo, and Knivsta in Uppsala County, north of Stockholm County.
Since the establishment of the Mobile Team in September 2011, fewer older patients visit the emergency room at Uppsala University Hospital. The Mobile Team started as a pilot project, which became a permanent unit in Uppsala, in January 2014.
Uppsala University Hospital is the only hospital with an emergency room in Uppsala County. Uppsala University Hospital is a public hospital financed by county taxes. Fewer visits to the emergency room thus save costs for the county. One visit to the emergency room is assumed to cost the county hospital 2,500 Swedish kronor (350 US dollars)[1]. In a conversation with the Mobile Team, one of the team’s two physicians, Magnus Gyllenspetz, explained to me that Uppsala County saves costs if the team makes three home visits per day. The savings come from reductions in the number of ambulance trips and the number of treatments provided in the hospital.
The total yearly cost of the Mobile Team is 3.5 million Swedish kronor (five hundred thousand US dollars). Uppsala County saves 2.5 million Swedish kronor (350,000 US dollars) on reduced outpatient treatments of the elderly alone. The largest savings are in the area of reduced hospitalizations for this group. Estimates for 2012 indicate that the Mobile Team saves Uppsala County over nine million Swedish kronor (1.2 million US dollars) annually on inpatient treatments for the elderly, excluding the costs of the Mobile Team.
Without the Mobile Team, an estimated 460 patients would have traveled to Uppsala University Hospital for treatment during the pilot phase, from September 2011 to January 2014. These 460 patients are “avoidable inpatients,” patients who can avoid a stay in hospital with treatment or social care assistance at home.
Apart from the economic benefits, patients like the Mobile Team. Fewer patients need to travel to the hospital. Fewer patients need to wait in emergency rooms. Fewer relatives worry about the health of their elderly loved ones. Fewer relatives must take time from work to help their relatives get to the emergency room. The Mobile Team cares for the ill residents in nursing homes. Because ill nursing home patients are the responsibility of the Mobile Team, the nurses in the nursing home are able to continue to care for all of their patients. If the nurse from the nursing home had to travel with the resident to the emergency room, then that nurse could not care for other patients.
Considering all the benefits, why is there only one Mobile Team with this setup in Sweden? Why do some older patients who need urgent care still travel to the emergency room? Is the Mobile Team too good to be true? How can we explain the fact that there is only one Mobile Team financed by a municipality and a county in Sweden?
There are many answers to these questions. Some older patients feel safer in emergency rooms. Most patients want the freedom to choose where to obtain treatment, at home or in emergency rooms, and some older patients feel safer in emergency rooms. People do not like to be told what kind of healthcare is best for them. Some simply do not know about the Mobile Team. Healthcare personnel follow routines. Some employees of the county do not work with the Mobile Team simply because it is not part of their routine. In my conversation with the five members of the Mobile Team, they expressed a desire to develop a new promotional strategy that would help the team reach out to more patients and partner organizations in the county.
The Mobile Team in Uppsala became a permanent unit one year ago, on January 1, 2014. I hope that other municipalities will establish Mobile Teams in the future, as more people become aware of the many benefits a Mobile Team can bring.
This is a happy thought for the New Year.
Happy New Year to all readers!
[1] “Final Report on the Mobile Emergency Team for the Elderly, 2013”. Author of the report: Swedish Association of Local Authorities and Regions (Slutrapport för projekt kring de mest sjuka äldre Mobila hembesöksteamet i Uppsala, SKL)
The Mobile Emergency Team for the Elderly

The office of the Mobile Emergency Team for the Elderly. Here, a nurse and a physician prepare to start the day by checking emails for updates on any of their patients.

Pia, one of the team nurses, leaves for a patient visit. She brings all the equipment she needs to treat patients at home.
Last week, I traveled to Uppsala from Stockholm to meet the team of the Mobile Emergency Team for the Elderly (Mobile Team). I am in the process of writing an in depth case study of the Mobile Team. This case study is part of our larger effort to identify good practice in integrated eldercare in a number of countries, including Sweden, Singapore, and the United States.
The Mobile Team is a leading example of integrated eldercare. Healthcare professionals can learn from the organization in general, and from its philosophy. As I build this case study, I will share with you some of my experiences with the process and what I am learning. In a series of blog posts, I will tell you about the Mobile Team and highlight different aspects of their work.
The Mobile Team started as a project in 2011, with financial support from the Swedish Association of Local Authorities and Regions. Today, the Mobile Team is financed by Uppsala Municipality and the Uppsala County Council. Uppsala County is located just north of Stockholm County. All members of the Mobile Team are employed by Uppsala County, which covers sixty percent of the total costs of the Mobile Team. Uppsala Municipality covers the remaining forty percent of the costs. Both the county and the municipality raises funds through taxation.
The Mobile Team becomes involved with patient care through several different avenues: Nurses who work in homecare organizations contact the Mobile Team when they need a second opinion on a patient. Employees at care homes for the elderly contact them for advice. And ambulatory personnel coordinate their efforts with the Mobile Team.
The Mobile Team centers on the needs of the patient. The objective of the Mobile Team is to offer urgent care at home to people over the age of sixty five. Many older patients visit emergency rooms at hospitals for urgent but non life threatening care that can be treated at home. Often, these patients must wait for hours at emergency rooms because their illnesses are not as pressing as the illnesses of other patients seeking emergency care.
The Mobile Team performs urgent care right in patients’ homes. The Mobile Team is able to measure glucose, take blood tests, test urine, and perform electrocardiograms in the home. The team can treat patients with a range of drugs at home. They measure blood flow in arteries to assess if the blood circulation provides enough blood to the legs and to the brain. Blood circulation to all tissue is necessary to avoid stroke, for example. The team also measures saturation, or oxygen levels in the blood.
They treat patients with pariboy, an inhaler, if patients experience difficulty breathing. The team also treats minor wounds. When a patient needs treatment at the hospital, the Mobile Team coordinates with the ambulatory service to arrange transport.
Many older patients need support at home from multiple caregivers. The Mobile Team coordinates care with these caregivers, including professional homecare providers. If a patient visits the emergency room for an illness that can be treated at home, a municipal nurse of the Mobile Team, who works at the hospital emergency room, informs the patient of the Mobile Team. If possible, the municipal nurse informs the patient caregivers of the treatment that the Mobile Team can offer at home. If a patient needs urgent care a second time, the caregivers and the patient know about the Mobile Team.
The Mobile Team includes a nurse from the municipality and a doctor from the county. Sometimes, the municipal nurse needs assistance from the doctor to treat patients at home. In turn, the doctor often relies on the expertise of the municipal nurse about the full care plan for a particular patient. For example, the municipal nurse coordinates the effort of the Mobile Team with the effort of homecare teams. The Mobile Team and homecare teams work together to ensure that patients obtain the support they need to stay at home and recover. Both the healthcare and the social care needs of the patient are assessed. Many times, doctors assess healthcare needs in isolation. Homecare teams assess social care needs. The Mobile Team can help provide for these needs by increasing communication between caregivers.
The quality of healthcare delivered to a patient depends to a large extent on the quality of communication between caregivers. This is particularly true for older patients with complex needs. The municipal nurse in the Mobile Team can update homecare providers on new treatment and new medications. Sometimes, the communication between doctors from the county and homecare providers can become delayed. Since the Mobile Team only recruits nurses with experience from municipal care organizations, the nurses in the Mobile Team are familiar with the channels of communication in the municipality. This familiarity speeds up communication and creates added value to patients that obtain care from different caregivers.
The Mobile Team is a critical link in the integrated healthcare chain in Uppsala Municipality. The neighboring municipalities are examining the possibility of establishing similar mobile teams.
The combination of the medical expertise of the doctor from the county and of the network and the experience of the municipal nurse renders the Mobile Team more effective than its constituent parts. Integrated care requires that different care providers collaborate. Different healthcare providers must acknowledge each other, and they must understand each others’ abilities and limitations.
Healthcare professionals cannot become experts in isolation. High quality healthcare at home and the timely transfer of information to homecare organizations improve patient experiences and patient outcomes. The best healthcare at home will not in itself prevent the patient from falling ill a second time. A patient may need help cooking or remembering to take her medication. If the homecare team is not informed or fails to help the patient take her medication, the patient may soon fall ill again. This is just one example of the interdependencies of integrated care models. Each care provider depends on other care providers. Patients depend on multiple care providers.
The Mobile Team collaborates with nursing homes, ambulatory nurses, the emergency service at Uppsala University Hospital, and various homecare organizations. Follow this blog for more information about how the Mobile Service works with other healthcare providers.
Nobel Week Dialogue
This week is a special week in Stockholm. The Nobel Laureates of 2014 have come to Stockholm for a week full of events. Some of the events, like the Nobel Week Dialogue, are open to the public. This year, the topic of the dialogue was aging, so I could not stay away. I would like to share some of the impressions from the Nobel Week Dialogue.
I listened to the panel “Diseases of Aging.” For information on the panelists and to view the program of the Nobel Week Dialogue, please visit the Nobel Week Dialogue website.
The panelists and the audience discussed how the burden of disease changes as our population ages. More people suffer from stroke, from cancer, and from cardiovascular diseases. Many older people suffer from several diseases at the same time. One disease, such as obesity, is a risk factor for other diseases. Can we afford to treat these diseases in the future? Are there effective ways to prevent these diseases?
You can watch the panel discussion here. The discussion yielded some useful insights: We have not slowed the development of age related diseases like dementia. We have postponed the onset of age related diseases. We do not age more slowly. We age later in life.
When we stay physically active, we help our bodies and our minds to stay young. When we remain socially connected, we slow down the aging processes. When we learn, we activate parts of the brain that prevent us from aging. We ought to remain students throughout our lives.
Some age related diseases have common causes. If we can identify the common causes, we can prevent or delay several diseases at the same time. Once a person develops diseases, we must treat each disease separately. Professor Miia Kivipelto, a geriatric epidemiologist at the Karolinska Institute, argued that prevention is partly a political issue. We must make it easier for people to lead healthy lifestyles. Linda Partridge, Director of the University College London Institute of Health Aging, disagreed. She argued that raising taxes on unhealthy food would not prevent people from consuming sugary and fatty foods. We must persuade people to lead healthy lifestyles. We must educate people.
Professor Ingmar Skoog of the University of Gothenburgh highlighted another important point. He talked about early diagnosis. Most studies of dementia follow patients for a period of twenty years. What if the early signs of dementia are visible earlier than twenty years prior to the development of dementia? What if prevention as we see it today, such as exercise and cognitive training, are retarders of the disease? What if what we call prevention is not prevention? Perhaps we must understand the fundamental mechanics of the disease better. Perhaps we must learn how to diagnose dementia earlier than twenty years before the onset of the disease. Perhaps we must rethink prevention.
Sweden spends below five percent of healthcare costs on prevention, according to a recent report from the Forum for Welfare (Forum för välfärd). It is costly to screen people for diseases. We may need to screen one hundred thousand individuals to find the disease in one person who can benefit from an early treatment. The panelists and the audience talked about the importance of preventing diseases. What I missed from the lecture today was a discussion on cost effective prevention. The gains of prevention seem to be large. If we can reduce the costs of prevention, we could lower healthcare costs. We could offer early treatment.
The moderator, Göran Hansson, Professor at Karolinska Institutet asked the panelists if they believe we could repeat the success story of the reduction in smoking. Can we reduce obesity like we reduced smoking? Nobel Laureate Eric Kandel offered a positive view. We made it trendy not to smoke. Many people stopped smoking because it was no longer trendy to smoke. But Ms. Partridge countered with a pessimistic view. We were never made to smoke, but we were made to eat. Historically, the more we ate, the greater our chance of survival was. Evolution has equipped us with few tools to resist fatty foods. We have lived in abundance for a short period of time. Repeating the success story of smoking will be a challenge. Are you an optimist or a pessimist when it comes to reducing obesity in the world?
The discussions stimulated my curiosity. I want to learn about common causes of diseases related to old age. I want to know more about prevention of diabetes and early detection of dementia. The topics at Nobel Week Dialogue were relevant because the panelists discussed diseases that affect large groups of people. In Sweden, one hundred and fifty thousand individuals suffer from dementia, and two thirds of these people also suffer from Alzheimer´s Disease, according to the Swedish Dementia Register. There are over four hundred thousand individuals who suffer from diabetes in Sweden. And almost four hundred million people in the world suffer from diabetes, according to the International Diabetes Federation. These figures are growing.
I was happy to note that many young people attended the Nobel Week Dialogue. I am also grateful that Nobel Week Dialogue chose to focus on aging this year. ACCESS Health works actively to support young entrepreneurs who are interested in aging. Entrepreneurs in different countries participate in ACCESS Health incubator programs.
As previous authors of this blog have described, Modern Aging is an ACCESS Health project designed to encourage entrepreneurs to create new businesses to serve the needs of the elderly and the chronically ill. The Modern Aging project was first conceived and implemented in Sweden. Young entrepreneurs were selected to participate in a fourteen week educational program. The winner received money to start a company. ACCESS Health plans to replicate and expand the Modern Aging project in Europe, the United States, and Asia. Check out www.accessh.org for updates on the program and the Modern Aging Innovation Laboratory.
Warm greetings from Sweden!
Sofia
Introduction
Hello everyone,
My name is Sofia Widén. I am the new coordinator of this blog. I joined ACCESS Health International earlier this month as a program manager. I am studying integrated elder care and healthcare. I will identify global examples of good practice in integrated elder care, together with other members of the ACCESS Health team working on elder and long term care. Some of the ACCESS Health team members will be blogging with me here. We have projects in countries as diverse as India, mainland China, Hong Kong, Singapore, and Sweden. We will tell you about our work on this blog.
Right now, I am based in Sweden, and I plan on working in the United States next year. I graduated from the University of Edinburgh in June 2014, where I studied economics, politics, and languages. In my role at ACCESS Health, I will be blogging about my research, about articles that I read, and about topics such as elder care and healthcare. From time to time, I will write about related topics. I love writing and I love reading. I will tell you about inspiring people that I meet. I will tell you about the exiting things that I learn through my research. Please send me comments and interact with me. Please follow me on Twitter @SofiaWiden, and check out our website www.accessh.org.
I wish you all the best and I hope that you will enjoy our blog!
Retirees on Speaking Exchange with Brazilian English students
Ideas sometimes seem so simple and obviously great, so you ask yourself ”Why has nobody come up with that before?!”
I came across the innovative Speaking Exchange project, which is about lightening up the lives of elderly, while at the same time giving Brazilian students the opportunity to practice their English skills. Reports about this case seem to go viral on the web these very days (see links below).
The idea was established by FCB Brazil, and put into practice together with the CNA language school in Liberdade, Brazil and the Windsor Park Retirement Community in Chicago.
I was so surprised and fascinated when I watched this clip about the Speaking Exchange:
The man shows the boy an old photo. “Is this your dad?” the boy asks. “No, It’s me and my wife when we were young”, he answers. “Oh you were good-looking when you were young”, the boy says – pause – “and you are still good-looking!”. 
“I look like I’m only 25”, another man says. He and the boy a are laughing, “but I’m 88”. The two are having a nice conversation. In the end, they share a big, virtual hug.
The school uses its own digital tool for video chatting where conversations are recorded and uploaded privately for teachers to evaluate the talk language-wise.
But there is much more to this than just the language…
It’s fun and warms my heart to listen to their conversations about all the World and his brother.
Read more:
Sensor Technology May Enable Successful Ageing-in-Place and, Concomitantly, Increase Value in The Process
As life expectancy and the proportion of people aged 65 and over increase, and integrated care and cost containment become a concern to many health organizations and policy-makers, technologies that utilize sensors to come up with new and innovative ways to support the elderly successfully age-in-place are increasingly becoming commonplace.
A flurry of new start-up health tech companies, mergers, acquisitions, and partnerships are entering the data analytics and sensor space to support seniors well-being. What once started as sensor networks in facilitated facilities and nursing homes are now moving into to every imaginable inanimate object in seniors private homes or apartments.
A recent partnership between Caremerge and Lively to create a platform to provide caregivers or family members with real-time alerts if something is wrong is one example.
Caremerge has a database of patient data from diagnoses, medications and allergies, and Lively develops passive movement sensors that can be placed in various spots in an elderly person’s home (i.e. the refrigerator, a pillbox, keychain, etc). So the cloud will be able notify caregivers when meals are eaten, medications are taken, if anyone leaves the house. More importantly, the platform can also notify caregivers if any disruption from a daily routine occurs. Although the partnership was announced relatively recently, they are in the process of taking in a few initial customers to test out their platform.
This business model is not unique for the vital sign monitoring and emergency detection space. Other similar ventures include: beclose, healthsense, and GrandCareSystems, among others.
Sensors to monitor vital signs need not be limited to being placed in inanimate objects. Research is underway to examine how to impant miniature sensors that can continuously monitor and report on a person’s health status.
Sensors introduce a whole wealth of data on patient behaviours that can be used to coordinate and integrate the management of care. So its no surprise that this space is seeing a lot of investment growth from traditional investors, but also from a growing number of large hospital networks and non-health IT companies.
The increasing trend in sensors and smart technology suggests that being monitored-all-the-time may soon become the norm for the elderly as they age. It may even spread to the non-elderly after, as “Smart homes” may become standard.
The applications for sensors to enable successful ageing-in-place seem limitless!
With more than $7.4 billion for over 1,393 deals occurring in the Health IT space since 2010, according to Startup Health, it would not be far-fetched to expect more excitement and innovations in this area very soon.
Sources:
http://www.nibib.nih.gov/science-education/science-topics/sensors
Portraits of elders
Beautiful photos of elders. It’s rare that we see these. We spend a lot of time talking about ageing and elders, but we rarely highlight the beauty of years of laugh lines, eyes that have seen generations grow, and skin that has truly weathered the storms. Ageing is beautiful, and the photographer Danny Santos II depicted it when he photographed seniors for Project Silverline, an initiative by SingTel to put refurbished iPhones in the hands of seniors, to enhance their interactions, their health, and ease the sense of isolation many elders feel. To see the photos that Danny took of seniors in Singapore, click here.
Modern Aging: inBelly

Today’s blog post is written by Kristina Saudargaite who is the founder of inBelly. This organization is already helping children at schools to have better food by identifying and classifying additives. Now, inBelly wants to branch out to another sensitive target group, the elderly. Read Kristina’s story here:
My name is Kristina Saudergaite and I love food. I love eating, cooking, going to the grocery store etc. I also love knowing what I eat. For this purpose, my friends and I once looked at the ingredient list. We saw many chemical names that we could not understand or tell how they affect our health. Thus, we checked.
The results shocked us! Commonly used E250 is classified by the International Agency for Research on Cancer as probably carcinogenic to humans or in simple words it is likely to cause cancer. E211 or sodium benzoate is not harmful on its own; however, it reacts with vitamin C and releases benzene – a known toxin. And who does not eat products often containing E211 such as shrimps together with a slice of lemon or maybe drinking Must with a salad
These are only a few examples; but food is increasingly stuffed with chemicals and this puts our health at risk.
The amounts of additives that may cause adverse effects are regulated by the EU. The problem lies in the fact that tests are made on healthy individuals (or animals). However, sensitive subgroups such as the elderly may be much more susceptive to the additives and adverse health effects related to them. Nursing homes do not have enough information to make sure that the food they buy do not contain harmful ingredients.
inBelly has the expertise and a rigorous database on food additives. Moreover, we have a technological solution that enables to quickly check if a product contains anything harmful.
In Sweden we have found many food products containing additives banned in other countries, such as Canada and/or linked to diseases. This knowledge exists in academia and in public documents but since the information is presented in a complicated and scattered manner, it rarely reaches the wider public. inBelly is unique since it uses official and scientific information about food additives and depicts it in a non-scientific “easy-to-understand” kind of way. The app simply shows a sign indicating that the scanned product contains additives banned in other countries. Our service innovation lies in using a mobile solution to translate knowledge from academia into simple visual signs in order to make the information quickly and easily available to everyone. With our mobile app people can scan barcodes and get information whether this particular product contains any ingredients that may be linked to diseases. The initiative won the Stockholm Innovation award in the service category 2012.
We are currently using this knowledge to help pre-schools to choose better food. We are cooperating with the chef at Globala Gymnasium to go through the products they purchase and analyse if any of them contain additives that may be harmful. This helps the institutions to ensure better food.
Since the elderly, similarly to children, is a sensitive group, we plan to offer our services to help nursing homes to go through the food they serve the elderly and check if they contain harmful additives. This would ensure good quality food and best possible health and wellbeing for the elderly.
Follow inBelly on facebook.com/inBelly or on Twitter @inbelly_guide
Source: http://www.socialinnovation.se/sv/modern-aging-blog-inbelly/
Modern Aging: Cross-generational housing

Three young women have come up with an idea that solves two problems with one solution; social isolation among elderly and shortage of housing for students. Here is their story;
Gabriela, an economist from Czech Republic; Bibiana from Colombia with higher education background in political science and Kika from Spain with higher education background in history. Although each of us had different reasons to move to Sweden, our interest in entrepreneurship and innovation in the social sector brought us together.
Daily, we encounter people around the city that even though they are senior they manage to live independently by themselves. At first, we were positively surprised by this, but when we looked closer on the psychological and social factors that affect the health and quality of life among the older people, we realized that loneliness is one of the most important problems within this population in Sweden. A problem that becomes very costly for society in the cases where it leads to depression, additional to the obvious personal suffering for the people being lonely.
Our innovation is to develop a tool to identify and match older people living alone and having a spare room in their homes with students in need of accommodation in Stockholm. Our project is called Tillsammans, which means Together in Swedish. It is a simple solution with the potential to enrich the lives of both students and elderly by creating daily inter-generational meetings as well as saving money for society.
Our project will use already existing resources; contribute to the social cohesion and strengthen the social networks.
We are aiming to find partners from the elderly care sector, pensioners’ organizations, universities and any other interested in improving the lives of the elderly.
Being part of the Modern Aging program gives us a unique opportunity to meet entrepreneurs, mentors and professionals from the S
wedish health care sector. Thanks to the network of those professionals and their intensive coaching we are building a concept around our idea and turning it into reality.

Source: http://socialinnovation.se/sv/modern-aging-blog-tillsammans/
http://homeshare.org/picture-library/austrianimage_austria-bmp/
Modern Aging: Ask for Answers

This week’s Modern Aging blog post comes from an American medical illustrator with a passion to improve health communication for elderly through visual media. Please read about the digital tool she is developing:
“I am excited to share with you an idea I have been developing as a social innovation for the elderly in health care. Today I will tell you about myself, and why I am considering the health needs of the elderly in Sweden. I will introduce the problem needing attention and how I propose to tackle it. Finally, I will let you know how you can connect with me if you would like to be part of this dialogue!
So who am I, and what brought me to Sweden? Well, my name is Anneliese, and I am an American citizen with Swedish heritage from both sides of my family. In 2010 I traveled to the “motherland” to see where my farmor, and my mormors parents came from. While visiting, I bonded with new friends and distant relatives, but visiting with relatives from my grandparent’s generation over fika was particularly special for me. During that trip I decided I wanted to come back to Sweden to study and experience more of Swedish society.
While back in the US making plans to return to Sweden, I was witness to the failing health and death of my mormor, Anna, and morfar, Winston. Winston lost his life, at 93 years of age, as a result of Alzheimer’s. While Anna, who suffered from morbidities common in the elderly, died only a few months after at 91 years. These experiences with my own family helped me to realize many of the challenges facing our aging global population. Now, I look to apply my education, work experience and research to help address these challenges.
My recent research has focused on the communications between patients and their care providers. The clinical setting can present many communication barriers, including a power dynamic between the patient, with limited knowledge, and the care provider, with greater knowledge. For the elderly, dementia, learning style, literacy and language skills can also contribute to communication barriers they face when determining their health needs. Further, many elderly patients have an increased number of health appointments where they might struggle to remember what to ask their care provider, or may not be aware of the proper questions to ask. Additionally, they will need to remember details communicated to them after an appointment. If not recorded, these details can be easily forgotten. My solution is simple, “Ask for Answers.”
Ask for Answers is a media based tool (web/app), which aims to arm the aging population with the questions they should have available when visiting a health provider. The questions target their specific communication needs and are broken down by medical specialties to be more effective. Patients can use the electronic interface to access their questions, type answers, exchange email with the provider, record audio of answers – which can then be transcribed, and even take photos of drawings or notes. The information would then be accessible later when the patient may have trouble recalling details from the appointment, or need to share them with another care provider.
Ask for Answers is centered on improving health communications between care providers and the elderly. It is a simple, user-friendly tool that focuses on enabling and empowering aging patients to better manage their health. With the aid of Ask for Answers, patient knowledge and satisfaction may increase, potentially resulting in improved health outcomes.”
Written by Anneliese Lilienthal
Source: http://socialinnovation.se/sv/future-of-elderly-care-may-be-answered-by-the-questions-we-ask/



























