Update From Modern Aging Singapore: Kickoff Workshop

Modern Aging Singapore kicked off in the middle of August. So far, the program has seen active participation and support from aspiring entrepreneurs. About three hundred students, health practitioners, researchers, and members of the public attended the Kickoff Workshop held at the NUS I Cube Building Auditorium on the morning of August 15.
Attendees were treated to four presentations from experts in aging and business: Overview of Aging by Prof. Angelique Chan of Duke-NUS Graduate Medical School, Healthcare and Business by Dr. Jeremy Lim of Oliver Wyman, Home and Center Based Care by Dr. Ng Wai Chong of the Tsao Foundation, and Product Design for Seniors by Hunn Wai of design firm Lanzavecchia + Wai.
 Prof. Chan highlighted some key trends and statistics on aging in Singapore. One surprising point was the high prevalence of social isolation among seniors here. This finding spurred aspiring entrepreneurs to think of novel solutions to address this trend.
Prof. Chan highlighted some key trends and statistics on aging in Singapore. One surprising point was the high prevalence of social isolation among seniors here. This finding spurred aspiring entrepreneurs to think of novel solutions to address this trend.
Dr. Lim went on to outline the aging sector in terms of business potential. One suprising finding, according to theNational Center for Policy Analysis, is the average net worth in 2010 was 848,000 USD for sixty five to seventy four year olds and nearly seven hundred thousand dollars for those above seventy five. These figures encouraged aspiring entrepreneurs to enter the aging sector.
Dr. Ng discussed the current status of home and center based care in Singapore. He highlighted specific needs in these care settings frequently used by seniors. This discussion allowed aspiring entrepreneurs to hone in on key areas of need and address these pain points. For example, some challenges in these settings include the quick and painless transferring of patients from bed to chair and vice versa, and increasing the time health practitioners can spend with seniors.
Mr. Wai rounded off the presentations with insights from product and design perspectives. He introduced examples of good design for seniors, such as mixed use canes and walkers, or stylish back braces. This presentation especially inspired aspiring entrepreneurs to consider seniors’ lifestyles and tastes when introducing new product ideas.
In addition to expert presentations, attendees also heard two senior role models share their life experiences and lessons. Younger members of the audience seemed glad to hear the wise advice dispensed by the seniors. The kickoff event concluded with a networking lunch. Participants became so engrossed in conversations around aging that they lingered past the scheduled end time.
Currently, Modern Aging Singapore has progressed to the business curriculum and selection phase. The top twenty teams have been selected and paired with industry mentors to hone their business ideas. The twenty teams will soon be pitching at the semifinals judging event for the top six spots. Meanwhile, all participants of Modern Aging Singapore are able to access the same business and aging curriculum on the Modern Aging Online Learning Portal to continue learning and improving their business ideas. If you would like to access the Portal, please write an email request to info@modernaging.org.
Find out more about Modern Aging, at www.modernaging.org.
US House of Representatives Votes to Repeal Medicare Sustainable Growth Rate and Strengthen Medicare Access

The United States Capitol Building. (Photo: House Press Gallery)
We at ACCESS Health have been watching the news closely for the last two weeks. The issue of interest was the vote by the United States (US) House of Representatives on March 26 to repeal the Medicare sustainable growth rate formula and to “strengthen Medicare access by improving physician payments and making other improvements.” The bill can be viewed here.
This event is noteworthy in a few ways. One is that the 392 to 37 vote reveals overwhelming bipartisan support for these changes. Another is that, if passed by both houses of Congress, the bill would change the US healthcare payment system significantly. The bill still needs to be passed by the Senate.
If passed, how will the bill affect healthcare in the US? First, the bill repeals the sustainable growth rate formula used by Medicare. The sustainable growth rate formula pegs provider reimbursements to economic growth, as measured by gross domestic product (GDP). In place of the sustainable growth rate formula, the bill proposes value based payment models such as accountable care organizations and bundled payment. Accountable care organizations link doctors, hospitals, and other health professionals together to develop tailored care plans for Medicare patients. These care plans encompass the entire care process, matching the appropriate service to patients’ needs and reducing duplication of efforts. The bundled payment system reimburses care providers based on expected costs for specific clinical issues. This prevents unexpectedly high costs for patients.
Presently, the US healthcare system uses a fee for service model to pay providers. This means providers are paid for each individual service or operation, regardless of necessity or efficacy. As described in Forbes, “[Fee for service] actually rewards providers financially when patients suffer complications or infections, and pays them more if [providers] order unnecessary tests or procedures.”
Changing this system would remove incentives for healthcare providers to push large numbers of services on patients. Replacing fee for service with value based payment models could improve patient outcomes while reducing costs.
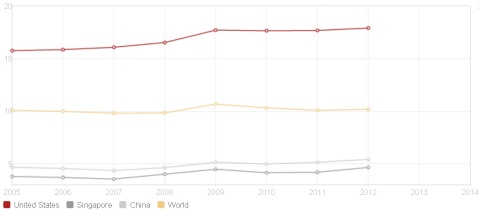
Spending on healthcare as a percentage of GDP in the United States, Singapore, and the world. (Picture: World Bank)
In the future, the high percentage of GDP spent on healthcare in the US may fall. According to World Bank data, the United States spent nearly eighteen percent of its GDP on healthcare in 2012, the highest in the world. GDP savings on healthcare would allow higher spending in other areas, such as education.
However, it is still too early to tell whether the bill will pass the Senate. In addition, there are still many challenges to the change. Many healthcare providers still cling to fees for services models of payment. It is also challenging to define key performance values for providers. Will providers aim to reduce readmission rates or improve life expectancies of patients? At this point, performance values are not standardized. Nevertheless, the strong bipartisan support for the bill shows a consensus that the existing sustainable growth rate model is undesirable.
This movement represents a move toward a capitation payment system, which pays providers a set amount for each patient, regardless of service type. Capitation systems are used by countries like Italy, the United Kingdom, and Denmark. In addition to the US, fee for service is used in countries like Japan, Germany, and Canada.
Interestingly, China has used the fee for service system since the 1980s. China has experienced healthcare cost increases, poor quality, and a questioning of medical ethics. These factors have led to experimental healthcare reforms, since the 2000s. City and local governments were encouraged by the central government to redesign the healthcare system, with wellbeing of patients as a main goal. China tried bundled payment systems, with some success. Jining saw a thirty three percent reduction in expenditure, while Shanghai saw a seven to twelve percent reduction in cost per outpatient visit. However, these initial results are not conclusive of the superiority of a capitation system. China continues to experiment with and review healthcare reforms.
If the US moves forward with the repeal of the sustained growth rate for Medicare, other countries facing challenges with fee for service healthcare models may follow suit. The ripples of this bill are potentially larger than domestic US healthcare policy. What do you think of these policy developments? Tell us your thoughts by leaving a comment.
Technology and Aging: Read the Interview and Learn what the Elderly Want!
ACCESS Health studies good examples of elder care in Sweden. In a series of group interviews, the Swedish team of ACCESS Health meets with a group of senior citizens to understand their needs. In this interview, the participants discuss technology, share their views on Swedish healthcare, and tell us about their experiences as informal caregivers. When they learned about the work of ACCESS Health, the participants volunteered for the focus group. The focus group participants live in the city of Eskilstuna, one hour southwest of Stockholm.
The blog post of this week is an extract from a group interview conducted on December 31, 2014 with Gudrun Bergström, eighty six, Gujje Byström, eighty nine, Inga Brehmer, eighty eight, and Ingrid Svahn, eighty five.
This is an insightful and fun read! Enjoy!

Participants of the ACCESS Health technology focus group. From the left: Inga Brehmer, Gudrun Bergström, Ingrid Svahn, and Gujje Byström.
Interview
Inga Bremer (IB): My name is Inga Bremer. I am eighty eight years old. I am interested in technology. I own an iPad. I own a Doro telephone. [Doro is a company that developed a simplified mobile telephone for older users.] My Doro is easy to use. My Doro telephone is not a smartphone. Dora does develop smartphones for older consumers right now. I also own a laptop. I own other technical devices at home, such as a dishwasher and a washing machine. I also have a small automatic vacuum cleaner so that I do not need to vacuum constantly. I have three large flat screen televisions with over fifty channels. I would call myself mildly interested in technology.

Inga Brehmer shows her Doro telephone and her tablet, which she uses to listen to the radio, to view emails, and to take pictures.
Gudrun Bergström (GB): My name is Gudrun Bergström. I am eighty six years old. I love technology. I am handicapped. I have poor eyesight. Technical solutions help me live with my sight impairment. I do not own a smartphone. I own a Doro telephone.
I have one of the newest stationary computers that you can buy. I use a magnifying software program that helps me increase the size of the text of the documents on my computer. I own an external hardware product. This hardware product helps me to magnify texts and images so that I can read and see the images better. This program is called Zoom Text.
I wear a watch that reads the time for me out loud. That is a great device. I have hearing aids. I also have three televisions. I use my three televisions. I have connected my television in the kitchen with an external hard drive so that I can record programs and store them.
Sofia Widen (SW): Do you record a lot of television programs?
GB: Yes. It allows me to watch them when I want to watch the programs. It took some time to figure out how to record programs. Learning is a gradual process.
I buy technology products. The booklet with instructions is written in a small text. This is problematic. It is difficult for older consumers to read small text. I can read instructions with my magnifying program. My dream is that doctors will find a way to operate a new sight nerve into my eyes so that I regain my sight. We are not there yet.
SW: Do you use your computer to browse websites?
GB: I browse a lot of different websites. I disapprove of some things that people write on Facebook.
SW: Do you have a Facebook account?
GB: Of course. I am on Facebook.
SW: Are you active on other social media sites?
GB: No. I am not interested in blogging or in tweeting. I use Skype. I Skype with my family. I have a wireless internet connection in my apartment.
IB: We should have spoken before you, Gudrun. You have so many devices.
GB: I love technology. My husband was not interested in technology. I installed devices at home. I learn about new products. I want to buy them. More people my age ought to take an interest in technology. Technology can help the elderly.
Ingrid Svahn (IS): Technology is in your nature. Either, you understand technology or you do not.
GB: I disagree. Look at the young who adopt technology. Are they born with an ability to absorb technology quickly? I do not think so. The young set aside time to learn how to use the technology.
IS: My name is Ingrid Svahn. I just turned eighty five. My husband knew everything about technology. I never needed to learn. My husband passed away a few years ago. I use modern technology. I am not interested in technology. I had a computer. I threw it out when it crashed.
SW: What did you use your computer for?
IS: I served on the board of an organization. I used my computer to type out the minutes from our board meetings. I have a smartphone. I use my smartphone sometimes.
SW: How do use your smartphone?
IS: I play games. I like Alphabet and Scrabble. I will say, though, that like other retirees, I do not have time to play all these games. Many retired people I know say they are busy. I also feel that I am busy all the time. I also own televisions. I use a dishwasher and a vacuum cleaner.
I use a pen for my touchscreen smartphone. I do not have Wi-Fi. I access the internet through the mobile network. Other family members discuss what kind of technology I need. They discuss whether I should install Wi-Fi or not. I do not know how the discussion will end. I might buy a tablet.

From the left, Inga Brehmer with her Doro telephone and her tablet. In the middle, Gudrun Bergström, with her Doro telephone and her tablet. To the right, Ingrid Svahn with her smartphone.
GB: I recommend a tablet. Tablets are great. You can carry it around. You can carry a mobile phone of course. I would not compare the two products. A tablet is helpful for my reduced sight. I prefer a larger tablet.
Gujje Byström (GBO): I am eighty nine years old. I am not interested in technology. I own one television. I watch eleven channels. I dislike watching television during the day. I record my programs. I watch them in the evening.
From the left, Inga Brehmer with her Doro telephone and her tablet. In the middle, Gudrun Bergström, with her Doro telephone and her tablet. To the right, Ingrid Svahn with her smartphone.
GBO: I use hearing aids. I use a walker. The walker helps me when I shop. I can carry a lot of bags. I hang them on my walker. People pestered me to get a walker. I think it is wise to wait until you really need a walker before getting one. You become dependent on your walker. I could not manage to carry my groceries without my walker.
I prefer to use a cane. I have a beautiful cane. I like my cane. I have had hip and knee surgery. After my surgery I decided to get a cane. There are flowers on my cane.
IB: I have a cane. My doctor prescribed the cane, so I obtained it for free. We buy technology such as canes and walkers. We buy them because we want nicer versions. In Sweden, you obtain technical aids from your doctor or from your municipal care organization. The devices are almost free or charge. You pay up to a fixed sum every year. This is a low sum. If you pay the fixed sum, you can obtain all devices that you need.
GB: We can discuss if you always obtain all the devices and all the aids that you need. I have a friend who requested two walkers. She was refused those two walkers. She wanted one robust walker for outside use in the snow. She wanted a smaller walker for use inside her apartment.
I returned the walker I was given for free. I bought my own walker. Look at my walker. I can lift it. It is light. [Gudrun demonstrates. She brings out her walker to the focus group.]
GBO: Those walkers are expensive. You made an investment.
GB: I can carry up to seven bottles of wine with this walker!
SW: Can you use the walker with thin wheels outside in the snow?
GB: If it is that snowy I do not go outside. There is no reason for me to leave the house when I cannot walk on the streets. Most Swedish cities are not accessible to the elderly in the winter. Too much snow and ice on the pavement prevents the elderly from leaving their houses.
Södermanland County Council hands out two types of walkers: one with large wheels and one with smaller wheels. Rules vary from county to county because regional governments are autonomous. The number of aids that you can obtain from each county varies.
GBO: The design of certain walkers can hurt your shoulders. I experience pain in my shoulders because of the way I walk and what I carry. I never experienced pain in my shoulders before. I have experienced pain in all other parts of my body before. I never suffered pain in my shoulders before.
You will soon be able to read the entire interview, posted on the ACCESS Health website here.
TioHundra – A New Integrated Care Model for Sweden?
This blog post introduces Care Company TioHundra in Norrtälje, Sweden. This is a unique model of integrated care in Europe. I have had the opportunity to interview Peter Graf, Chief Operating Officer of TioHundra. Peter Graf talks openly about the challenges and the many opportunities that TioHundra faces. I have also had the opportunity to interview members of the staff and managers throughout the organization. Through these interviews, I have gained an understanding of the different parts of the company. I will tell you about my impressions of TioHundra in a series of blog posts. You can access the full interviews and all relevant background information from this case study on the ACCESS Health website.
Background
An older person with multiple diseases often requires care from several healthcare and care providers. This elderly patient may travel to a local hospital for treatment. It is not uncommon that up to sixty people from various care organizations are involved in the care of an older individual with complex care needs. Patients with complex care needs require the services of both the county healthcare providers and the local municipal care organizations. As individuals in Sweden age, and as more people live with multiple diseases and have complex care needs, counties and municipalities realize the need for greater care coordination. Care coordination to meet the needs of the elderly is one of the greatest challenges in Swedish healthcare, witnessed by the large effort of the previous center right coalition government to improve care coordination in the program “The Most Ill Elderly” from 2010 to 2014.[1] The previous government allocated over four billion Swedish kronor to improve the coordination of care for the most ill elderly. TioHundra shows that their model of integrated care already works well. During the program The Most Ill Elderly, TioHundra received funding based on the results they displayed in their work for the most elderly ill. These results included a reduction in unsuitable medication for the elderly and shorter wait times in the emergency room, among other areas.
Elsewhere in Sweden, regional governments manage the healthcare provision while local governments provide homecare and social care. Well defined areas of responsibility ensure that each provider in healthcare and in social care can focus on a range of services. In theory, the specialization of each level of government ensures that citizens obtain the healthcare and homecare they need. In practice, the division of responsibilities causes delays in service delivery, and at times, it compromises the quality of care. Regional and local governments use different communications systems, have distinctive work cultures, and use individual terminologies. Older frail patients, among other groups, suffer when healthcare providers fail to communicate effectively across organizations. TioHundra overcomes many problems of care coordination. Instead of coordinating care across organizations, TioHundra merged multiple care providers, now operating as one large healthcare and care system. This merger entails one of the largest regional reforms of Swedish healthcare since the Nobel Reform in 1992.
Care Company TioHundra is a public healthcare company that provides integrated care in Norrtälje, a city one hour north of Stockholm in Sweden. TioHundra operates an emergency hospital, six primary healthcare clinics, and a home healthcare organization for patients who are unable to travel to obtain care. It also manages social care and homecare organizations. The company runs nine nursing homes and it has 3,500 employees, including healthcare professionals and administrative staff.
To improve the quality of healthcare and to overcome the care coordination problems of regional and local administrations, Norrtälje and the Stockholm County Council established TioHundra in 2006.
Philosophy
The guiding philosophy of TioHundra is to construct an integrated healthcare system. The objective is to be the leader in integrated care in Sweden, and to be the number one choice of care provider in Norrtälje. The management approach centers on constant improvements. Managers and employees at all levels of the company identify areas for improvement, suggest new routines, and implement changes. The idea is to constantly improve service delivery and employee satisfaction.
Improved Care, Lower Cost
The ability to turn around negative operating results of previous years into a positive net result helped to convince politicians in the region that TioHundra improves the quality of care while lowering the delivery costs. Results from the employee survey show that the company employs a more satisfied workforce in 2014 than in 2013.
TioHundra manages to overcome certain problems of care coordination that persist in other regions and in other municipalities. Formal and informal channels of communication improve the transfer of information between different departments. Patient data is shared throughout the organization with the help of read only functions in patient journals. Weekly meetings of the management team foster an atmosphere of cooperation. Where disagreement occurs, the meetings serve as an arena for constructive debate.
Financing
TioHundra obtains one pool of financial resources from municipal and county taxes. Elsewhere, counties raise taxes for healthcare while municipalities raise separate taxes for social care. Budget silos prevent counties and municipalities to coordinate care in other parts of Sweden. One level of government is sometimes reluctant to deliver a service it considers to be the responsibility of the other level of government. The organizational structure of TioHundra allows this problem to be overcome through a lateral integration of caregivers from the county and the municipality.
Conclusion
In summary, TioHundra is a unique healthcare company. There are no other companies like TioHundra in Sweden. Few similar care organizations exist elsewhere in the Nordic countries. TioHundra reported a balanced budge for the first time in 2014. It also marked a year where management recorded improvements in employee satisfaction. TioHundra delivers healthcare of high quality at relatively low costs. The company has reduced the number of medications per older patient, reduced the prescription of unsuitable medications for the elderly, and it has shortened emergency room wait times for this patient group.
It remains to be seen how the integrated care model of TioHundra evolves. A transition in 2015 away from a focus on balancing the budget, towards operational and organizational changes is already noticeable. This is a young company with an eager management team. If the quality of care improves dramatically, and if the costs of healthcare can be contained in Norrtälje, other counties and municipalities may look into adopting the model of TioHundra.
[1] De mest sjuka äldre
Retirees on Speaking Exchange with Brazilian English students
Ideas sometimes seem so simple and obviously great, so you ask yourself ”Why has nobody come up with that before?!”
I came across the innovative Speaking Exchange project, which is about lightening up the lives of elderly, while at the same time giving Brazilian students the opportunity to practice their English skills. Reports about this case seem to go viral on the web these very days (see links below).
The idea was established by FCB Brazil, and put into practice together with the CNA language school in Liberdade, Brazil and the Windsor Park Retirement Community in Chicago.
I was so surprised and fascinated when I watched this clip about the Speaking Exchange:
The man shows the boy an old photo. “Is this your dad?” the boy asks. “No, It’s me and my wife when we were young”, he answers. “Oh you were good-looking when you were young”, the boy says – pause – “and you are still good-looking!”. 
“I look like I’m only 25”, another man says. He and the boy a are laughing, “but I’m 88”. The two are having a nice conversation. In the end, they share a big, virtual hug.
The school uses its own digital tool for video chatting where conversations are recorded and uploaded privately for teachers to evaluate the talk language-wise.
But there is much more to this than just the language…
It’s fun and warms my heart to listen to their conversations about all the World and his brother.
Read more:
Modern Aging ideas – new blog series

Our most loyal readers on Silverevolution may remember the program Modern Aging that we wrote about in April (see the post HERE). This innovation program for young entrepreneurs with ideas for the elderly kicked off in August this year. A group of 7 entrepreneurs have been selected based on the potential of their improvement idea as well as their motivation to lead the way in transforming the elderly care sector. We are currently in the act of developing their ideas with the help of mentors and coaches and in close discussion with the elderly themselves. During the next couple of weeks the participants will blog about their ideas on the Forum for Social Innovation Sweden and we will post them here on Silverevolution as well.
First in line; introducing himself and his idea is Victor Nordlind. This is his story:
One may ask why a person who is attending one of the world’s top hotel schools would want to pursue a career in developing and improving the elderly care. Most people expected me to walk in my father’s footsteps in the restaurant industry, rather than radically changing field to Elderly care.
But as I was required to carry out a feasibility study about an existing retirement home during my first two years at Ecole Hôtelière de Lausanne (EHL), I was given the opportunity to see the true potential within this industry. It encouraged me to apply for an internship within elderly care, which I am currently pursuing within Strategy and Business Development at Ambea Sverige, whose affiliation is Carema Care. For me, elderly care is an industry where innovation is necessary in order to provide the correct quality of life, which in my opinion is the meaning of hospitality.
When I first came across the Modern Aging program, I did not have a specific idea for elderly in mind. When developing the idea, it was equally important to link the project back to my studies, as to work with something that may truly make a difference within the elderly sector. I decided to contact a friend who has several years of experience within elderly care, and who is currently working in a nursing home here in Sweden. I was convinced that my determination combined with her extensive experience would bring something innovative out of the meeting.
As expected, we had a very interesting discussion, which brought several ideas to the table. Most of them were linked to the use of more technology, which is a frequently debated topic when talking about improvements within elderly care. The trend of using technology to improve efficiency is relatively new in the industry while it has been an essential part of the hotel and restaurant industry for years. More and more apps and other technical devices are being developed to simplify everyday activities for the elderly.
However, one question that came up during the meeting was “how can we use technology to better involve the caregivers within elderly care?” These professionals have valuable knowledge and experience, which they should be able to share easily. With today’s progression of social media and online forums, a place for caregivers and other health care professionals to meet online should be developed. There, they may share ideas, knowledge and ask questions to one another over space and time. This will not only simplify and streamline the daily work, but it will also improve the quality of care in nursing homes in the long run. A forum like this needs to be strictly confidential with only registered users permitted access. The idea is also that this platform shall be the forum that compiles and disseminates knowledge of the latest advances in medical, social and technological solutions for the elderly.
My current internship at Ambea combined with the Modern Aging program has helped me to better understand the current market as well as the future prospects of elderly care in Sweden. To date, Modern Aging has hosted several seminars and workshops carried out by inspiring guest speakers from various fields, such as young entrepreneurs, lecturers from top universities, and professionals from the public health care sector. With this promising start, I am curious and eager to find out where the program is going to take us.
“Digital Aging”: Trend II – Smart Home International Project
EU-funded unique international project aimed at providing safer and healthier aging is led by researchers at Örebro University (Sweden) in collaboration with twelve partners from six countries Sweden, Italy, Spain, Portugal, UK and Slovenia. The unique feature of the project is that it will provide seniors with smart home system combining both long-term health evaluation and caregiver-user interaction.
The project is called “Giraff” and received its name after remotely controlled mobile robot “Giraff” equipped with a display and loudspeaker. This robot lays in the heart of the smart home system in combination with continuous monitoring through a network of sensors.

“Giraff” system (to the right) enables communication between a senior and a caregiver while being at home
Multiple sensors are installed in the apartment and can measure blood pressure, body temperature and register movements. Data from the sensors will enable to identify if someone takes a sudden fall or doesn’t move for unusually long time, analyze sleeping pattern and level of physical activity, which can be of particular importance for physiotherapists. All the data collected from sensors are analyzed by an intelligent system, which is able to quickly alert the caregiver if something goes wrong and to conduct long-term health assessment of the seniors, thus giving caregivers a tool to adapt care plan to guarantee better quality of life.
Robot “Giraff” is designed for conducting virtual visits based on users need or on caregiver’s and family member’s intention to talk to the senior about his/her health measurements. “Giraff” can move autonomously around the apartment, find where senior is located or follow the senior around the apartment during “virtual” physician visit. In future, it will be senior’s decision on whether to use “Giraff” to have a virtual meeting with caregiver or make a journey to the healthcare center instead.
When it comes to privacy of health data, it will be only user who can allow access to health information for concerned family members or other caregivers. This will contribute to creating a user-friendly environment, where seniors will understand that they can receive an opportunity to improve their quality of life while feeling secure about privacy of their data.
The project has come to a testing phase in 15 real homes in Sweden, Italy and Spain. Last news tells about system installation in the homes of elderly women living alone in Malaga (Spain) and in Örebro (Sweden).
It is inspiring to see how modern digital technology can improve quality of life for elderly people! Stay tuned for future blog posts on digital technology for elderly care.
References:
http://www.giraffplus.eu/index.php?option=com_content&view=frontpage&Itemid=54&lang=en
Picture taken from:
http://www.oru.se/English/News/Smart-homes-technology-tested-in-Orebro/
“Digital Aging”: Trend I – Remote Home Monitoring
For the last decades, development of Information Technologies (IT) and sensor technologies has resulted in a great number of new services such as smartphones, tablet PC’s, wireless video games, robotics, Skype to name a few. With some delay in time these technology advances started to change the way healthcare services are delivered with areas of mhealth (using mobile devices for healthcare service delivery) and telehealth (delivering healthcare over distance) gaining wider acceptance. So now it is time to create a series of blog posts under the common name “Digital aging” to highlight solutions that are already available and can be used. Stay tuned to the next blog posts, if You want to know more.
One of the trends of applying new technologies is remote home monitoring of elderly people using a set of sensor devices and wireless data transfer. The main advantage of these tools is that it gives today’s active seniors and their families freedom, security and the ability to manage their health at home or away. Basic functionality of the remote home monitoring system can include:
- automated fall detection
- location tracking
- remotely managed two-way voice
- alert system
Additionally, some of the systems support integration with other health measuring devices and can track blood pressure, weight, blood glucose level and even transfer all these data to the patient’s Electronic Health Record (I will tell more about it in the later posts)
How it works?
A senior active citizen will wear a lightweight pendant everywhere he goes: inside the house, to the library, swimming pool, supermarket, park, etc. This pendant will be waterproof, easy-to-use and not necessary to be taken off even while charging and constantly serving as a part of a “Mobile personal emergency response service”, which will track the senior person movements, detect any case of possible fall and location of a senior and send alert to the caregiver/assistant.
As an example, Susanne, 82 years old, wants to live an active life and not be tied to her healthcare team, which includes her family and healthcare professionals. She wears a light device with her anywhere she goes. While walking in the park, Susanne feels dizzy and presses the help button on the device, thus initiating a two-way voice conversation with a support center. She tells about her condition and the support center assistant makes a decision, whom to send to help Susanne to get home safely. In case Susanne falls, the system will automatically track her location and an ambulance car will pick her up.
I believe such techniques are very inspiring and these types of solutions are already on the market with for example “GoSafe” and “Libris”. Moreover, in US, AT&T is offering “Libris” solution as part of a managed service for doctors and health insurers already. Why not set “free” both active seniors and their families?
References:
http://philipslifelinegosafe.com/new/
http://numera.com/platform-products/numera-libris
“AT&T and Numera Combine Personal Safety and Home Health management with New Personal Health Gateway”. Accessed at: http://www.att.com/gen/press-room?pid=23809&cdvn=news&newsarticleid=36052
Image : www.freedigitalphotos.net
2050 – Projecting the magnitude of demographic change worldwide
“I see old people” is how this chapter begins. I’m reading “The new North – The World in 2050” by Laurence Smith. Without having finished the book, I’m excited to share some of the thoughts. This chapter really struck me.

Smith is a young professor in geography and earth and space sciences at UCLA. In his book, he analyzes four key “megatrends” – population growth and migration, natural resource demand, climate change and globalization – and projects how our world could look like in 2050.
The world is filling up with old people. Smith begins by describing the four stages of the demographic transition, which is happening everywhere in the world: 1. High and similar rates of birth and death (e.g., the preindustrial era, with a small and relatively stable total human population); followed by 2. Falling deaths but not births (initiating a population explosion); followed by 3. Falling births (still exploding, but decelerating); and finally 4. Low and similar rates of birth and death (population stabilization at a new, higher total number.
He states that most OECD countries have now passed through these stages – except for those allowing high levels of immigration like the USA – and have stabilizing or even falling populations. Most low- and middle-income countries are still in stage 2 or 3 though.
Smith summarizes that urbanization, modernization, and the empowerment of women push fertility rates downward. In other words, the urbanization of society (if associated with modernization and women’s rights) helps slow the rate of growth (with exceptions). In low-immigration developed countries like Italy and Japan, and regions like Eastern Europe, populations are falling. Consequently, if fertility rates continue to drop as they are now, the world population might be around 9.2 billion in 2050 – the population will still be growing, but about half as fast as today.
One of the most profound long-term effects of women having fewer babies is to skew societal age structure toward the elderly. Of course, improving healthcare also extends our life spans. This aging will hit some places faster and harder than others. Today, Japan is the world’s most elderly country with a median age of 44.6 years. In Pakistan, in contrast, the median age is just 22.1 years. Korea, Russia and China will join Japan as the world’s geriatric nations. Korea, Vietnam, Mexico and Iran will age radically by fifteen years or more. Countries like Afghanistan, Somalia and the Democratic Republic of Congo will still have youthful populations in 2050. 
Smith asks: Is an elderly population a good thing or bad? He describes a possibly wiser and less violent society, which at the same time strains healthcare systems, and raises the economic burden on younger workers. The whole concept of “retirement” is about to undergo a major overhaul – people will have to work later in life. Big cultural shifts will be needed in the way we treat and value our elderly. Society must learn that aging and youth should be valued equally.
As the world grays, skilled young people will become a more and more craved resource, Smith concludes. Thus, those countries best able to attract skilled foreign workers will fare best. These young workers might come from Somalia, Afghanistan, Yemen, the West Bank and Gaza, Ethiopia, and much of sub-Saharan Africa, which will offer our world’s youth in 2050 based on current population structures.
Finally, the critical but open question that Smith poses is whether our poorest countries will be able to turn their forthcoming demographic advantages into the new skilled workforces needed to help care for an elderly world. This would require enormous improvements in education, governance and security. Women would have to start attending school and working in places where this is uncommon today. Terrorism would have to be sufficiently quelled. The countries that need young workers would have to accept immigrants from the countries that have them.
Hopefully, these things can be achieved.
PS: Check out Laurence Smith on Vimeo: http://vimeo.com/15715690
Innovating health through just-in-time evidence-based information
Hearing the term health care innovation, most people associate it with new technologies like robotic caregivers, digital imaging or breakthroughs in chronic disease treatment. The decision-making process towards the use of any of those innovative choices is based on the physician’s knowledge and experience.
“Healthcare innovation can be defined as the introduction of a new concept, idea, service, process, or product aimed at improving treatment, diagnosis, education, outreach, prevention and research, and with the long term goals of improving quality, safety, outcomes, efficiency and costs” (Omachonu et al. 2010). Thus, process innovations focus on improving quality of care for patients and enhancing health providers’ internal capabilities. However, innovation is difficult – the health field has rich evidence-based innovations, but they disseminate slowly, if at all (Berwick 2003). Six areas have been identified in making or breaking innovation in healthcare (Herzlinger 2006):
- Policy
- Stakeholders
- Funding
- Technology
- Customers
- Accountability
One opportunity to introduce innovation in healthcare is the use of evidence-based information, which is highly relevant to that particular patient – especially at the point-of-care. But how can the use of this kind of information be facilitated?
One tool that I came across is Elsevier’s ClinicalKey (www.clinicalkey.com). It is a tool that physicians can use to access evidence to make informed decisions at the point-of-care and throughout the patient journey. The ClinicalKey reference system links clinicians, medical librarians, and researchers to an online platform, which contains content from medical journals, books, multimedia, MEDLINE abstracts and other sources. Did you come across any similar tools?

To me, fast access to high-quality research evidence to inform decision-making in clinical practice is absolutely important for innovating – improving – health. What do we need to solve this?
Maybe we need harder, better, faster, stronger tools as such, but what I wonder more about is the role of stakeholders as the leaders in these processes. How can leadership for evidence-informed decision-making in health be encouraged? How to cure resistance to change and innovation?
References
Berwick DM (2003). Disseminating innovations in healthcare. JAMA, 289(15):1969-1975
Herzlinger RE (2006). Why innovation in healthcare is so hard. http://hbr.org/web/extras/insight-center/health-care/why-innovation-in-health-care-is-so-hard
Omachonu VK, Einspruch NG (2010). Innovation in healthcare delivery systems – a conceptual framework. The Innovation Journal: The Public Sector Innovation Journal, 15(1):2.
www.clinicalkey.com
http://www.youtube.com/watch?v=gAjR4_CbPpQ
Image: http://www.tcd.ie
Elders: Live independently without too much room for pride
The New York Times’ Personal Health blog included an article written by Jane Brody: “Staying Independent in Old Age, With a Little Help.” Here, the writer mentions how the majority of American elderly prefer to stay in their homes as long as possible. A barrier remains, however, as the homes they stay in are outdated relevant to the modernization of our people and the rate at which aging is increasing. Therefore, solutions are mentioned here — both on the house level and the community level — that may allow for elderly to live as independently as long as possible. House level solutions include the installment of grab bars, curbless showers, and the removal of steps. Community level changes include the provision of cluster housing in walkable communities within the vicinity of stores and public transportation.
While these solutions will help prevent social isolation and improve human elderly factors, one must also be aware of the signs of when one should consider moving an elder to a more supportive environment. These signs have been mentioned by Paula Spencer Scott, senior editor at Caring.com. Accidents, falls, diminishing health, slow recovery, inability to leave the house, not picking up the mail, not checking food expiration dates, fluctuating behavior, and increased loneliness are one of few signs to tell when the time may be right. Not only these, but if it takes considerable time and effort to care for this person and you are becoming affected if you yourself are the care provider, it is probably the right time to let him or her come to a place where he or she can be helped with a more constant environment of support. The question remains if these facilities will remain available in the coming future with enough staff. This will of course remain a concern and, to boldly say, should be a target addressed in all coming worldly or national health meetings of any kind.
—
References
How grandma celebrates Christmas by herself
I came across this article from the UK about elderly people spending their merry Christmas on their own. I found it interesting, depressing, and even discovered a link to health in the whole dilemma.
While for many people Christmas is the only time in the year when they actually meet family and friends, others are not cared for by anybody or do not care for anybody (anymore). Thus, they spend the celebration of love alone, like a quarter of all people in the UK that are older than 75 and live by themselves – even though the majority of them have children.
Experts say that “family breakdown is fuelling an epidemic of loneliness in old age” and that the fact that two in five marriages fail has serious impacts for the elderly. Young people have to divide their time between parents and step-parents. Besides, ‘silver separations’ are also becoming more common, with latest figures showing that more than 11,500 over-60s were granted a divorce in 2009.
In one of the largest surveys of its kind, the think-tank polled 2,000 over-75s to test how isolated the elderly truly are. ‘I’m 88 and I have nobody at all. I’m on my own’, said one, and ‘some days the only person I speak to is the boy in the shop when I pick up my paper.’
Growing isolation and loneliness makes elderly people particularly vulnerable – also in terms of health. Related mental and physical health conditions include a weakened immune system, sleep deprivation, higher blood pressure, a higher risk of dementia and depression. What to do?
In the UK there is an initiative that involves the police, fire officers conducting home safety checks, as well as social workers who see “warning signs” to connect people to local voluntary groups that can provide companionship. But is that a solution of the problem really?
——-
Chapman J (2011): 250,000 elderly people who’ll be spending their Christmas alone. Available: http://www.dailymail.co.uk/news/article-2078261/250-000-elderly-people-ll-spending-Christmas-alone.html#ixzz2FXDlyfWT
Let the cyber knife take away your pain
In 1983, the World Health Organization put cancer as a leading cause of death in South Korea. It has an immense impact with 64,000 people dying every year in Korea due to the disease. Luckily, the latest development in cancer treatment is available in Korea: Cyber Knife Radio Surgery. There are currently some hundred cyber knife systems installed in only few countries in the world. Korea was among the first to implement it and today, it has one of the most numbers of installed systems. Compared to UK and US, a cyber knife treatment costs less in Korea.
Cyber knife systems have been used to treat tumors in upper spine, head and neck since 1999 and in the rest of the body since 2001. John Adler invented the system for cancer treatment. It is made to deliver radiotherapy for malign and benign cancer tumors at all stages in specific parts of the body in a non-invasive way. It uses a real-time image guide to find tumors even if the patient is moving, and to deliver radiation with highest accuracy. It eliminates the need for invasive surgeries.
There are various benefits of the technique, e.g. faster procedures in comparison to other radiation methods, no requirement for hospitalization, no need for anesthesia and almost no post-operative care. Cyber knife surgery can even be used for tumors that have already received the maximum dose of radiation. There are no incisions or cuts, and recovery time is not needed. It can even be used for tumors in the spine, which are hard to treat because they are moving while the patient is breathing. The cyber knife can pinpoint the exact location of the tumor and beam into it without damaging other surrounding tissues. That leads to a shorter treatment period and a quick recovery. Treatment can be finished in less than five days on an outpatient basis, without spending a single night at the hospital.
One hospital in Korea is specialized in treating spine cancer. The oncology experts in Korea are highly trained and have years of experience in radiology and cyber knife cancer treatment. Medical staff in Korean hospitals are English speaking and communication will not be a problem when getting medical treatment there.
Cyber knife surgery abroad:
http://www.medicaltourismco.com/oncology/cyber knife-cancer-radiotherapy-overseas.php
Cyber knife Treatment for Spine Cancer
http://www.medicaltourismco.com/south-korea-hospitals/cyber knife-surgery-korea.php
The Rheumatic Crash of the Silver Wave

Rheumatoid Arthritis (RA) is a chronic condition that affects between 0,5-1% of the general population. It is considered an autoimmune disorder as the inflammatory system attacks joint locations of the body — typically in the hands but also other areas such as the feet.
Enough damage will considerably lower or possibly prevent the individual’s ability to perform motor activity.
Whether the inflammatory arthritides, including RA, have a distinct presentation and course in older as compared to younger subjects as first postulated in 1941 remains unsettled. The issue has gained significant importance as the proportion of the population who are over the age of 60 continues to grow in developed nations. As multiple newer treatment strategies emerge for RA, the efficacy and safety of these in elderly populations need to be evaluated as a distinct clinical issue.
— Aviva Hopkins, MD, and Carlos J. Lozada, MD
Traditionally, treatments known as Disease-Modifying Antirheumatic Drugs (DMARDs) have been used to treat RA in order to slow the progression of the condition — with methotrexate being the gold standard. In cases of heavy or severe inflammation and/or when DMARDs fail, glucocorticoids (corticosteroids) are also used in tablet or IV form. When used over time, these drugs cause considerable damage to the body. Immunosuppressives such as cyclophosphamide are also used in cases of strong inflammation and these drugs bear considerable toxicity — including the risk of developing infertility (which is vital to understand, especially considering the majority of cases are female; 3:1 in younger-onset RA). With these factors in mind, several new treatments have been made available and the most notable are called biologic drugs. These drugs are created from a biological process rather than being chemically synthesized; most often involving recombinant DNA technology to create, for example, monoclonal antibodies and fusion proteins. An example of a monoclonal antibody used in RA is rituximab, which was created as an “antibody” to specifically target B cells — which are a vital part of the immune response. Where a healthy immune system equates to a healthy person, in the case of an autoimmune patient the inflammatory response goes out of control and must be suppressed. Taking these drugs of course can lead to a rise in the rate of infections as they very effectively do what they were made for — lowering the immune response. However, a search on PubMed or any other medical database reveals a very positive force for the usage of biologic drugs; as they are also considered safer than some traditional DMARDs. Biologics have existed for approximately 20 years, but despite evidence showing them to be significantly more effective than DMARDs, they are quite costly. Therefore, biologics are typically reserved for those patients who do not respond well to DMARDs.
If there would be a way to make these biologic drugs more cost effective, these drugs are an important milestone for an answer to worldly health with the rising rates of elderly who may potentially develop RA. Novel drugs which may be considered similar to biologics have just been introduced within the past few years and these are known as protein kinase inhibitors. More research will show if these drugs will prove to be more cost effective than the competitive biologics.
References
http://www.cdc.gov/arthritis/basics/rheumatoid.htm
Science fiction medicine from Sweden
Imagine you were able to simply replace one of your organs once you fall sick. You just go to the hospital and quickly come out with a new intestine, kidney, liver or even heart, if an incurable disease was present. This sounds more like an idea from a science fiction movie than a like a feasible therapeutic option, but research on regenerative medicine and the engineering of “artificial” organs is happening to make these options a reality for many patients worldwide in the near future.
Nowadays, chronic diseases are a major health issue in almost every country – they cannot be cured and the patient’s best bet is to prevent those diseases and their complications. We are talking about e.g. diabetes, heart and kidney failure, hepatic disease and hypertension. After treatment has failed the last resort for many patients is organ transplantation. However, as simple as it may sound, there are countless complications involved, as the organ has to be compatible with the patient. The patient will have to remain on medication to lower his immune system response to the minimal for the rest of his life, which can make him more vulnerable to infections.
By the year 2010, over 90,000 people were signed in for the waiting list for a kidney transplant in the US and 3,000 at any given day for a heart transplant. Many patients who have no other choice of treatment wait, and most of the times death arrives faster than the suitable organ.
What if you could build a custom-made organ according to a patient’s need? A group of biomedical researchers at Karolinska Institutet in Sweden have pioneered what can be the first step in the beginning of a science fiction medicine: working with stem cells, which are cells capable of giving rise to any human tissue. They have managed to make a fully artificial trachea from scratch and implant it in a patient with cancer without any immunological reaction. The newly formed organ is built on a PET mold, yes the same used in bottles, which is as anatomically identical to the patient’s actual trachea – not only in shape but also in composition. The mold is filled with stem cells from the patient himself. Giving rise to a new and fully functional organ ready to be replaced.
The patient who went under this treatment is currently under annual checkups while living a normal life without health related restrictions. This is only the first step, but it is a firm step.
Thanks to Antonio Beltrán Rodríguez for sharing this post with our silverevolution-readers. Antonio is a biomedical student at Karolinska Institutet. Contact: antonio.beltran@stud.ki.se
And tomorrow WALL-E is taking care of you
 Nowadays, a lot of research is conducted in the area of healthcare robotics, which has the potential to increase the quality of life for our silver population. Imagine!
Nowadays, a lot of research is conducted in the area of healthcare robotics, which has the potential to increase the quality of life for our silver population. Imagine!
I would like to tell you about the examples of New Zealand and South Korea – two countries that are combining their knowledge in order to build and develop something groundbreaking. Here, South Korea contributes from the hardware-side, while New Zealand is busy developing the latest software (check out: HealthBots Project, launched in 2008).
Healthcare robots that can take grandma’s heart rate or blood pressure are the outcome of the research. But besides simple medical jobs, robots can also play a tremendous role in monitoring, as they are able to store and manage the patient’s relevant medical data. All this can make elderly care much more cost-effective.
Another idea is that robots can enhance old people’s quality of live by offering entertainment, e.g. through music, films, games and the use of social media as Skype.
——————-
All this sounds futuristic, but the question is if it is a concept that will be feasible: Will decision-makers be willing to invest in healthcare robotics? And will our grandparents (our parents? we? our kids?) enjoy interaction with robots? A lot more studies have to be carried out in order to find out more about cost-effectiveness, but particularly about interaction between human beings and machines – and thus, about the increase (or not) of people’s quality of life.
Healthcare robots could change lives: http://www.msi.govt.nz/update-me/success-stories/research/healthcare-robots-could-change-lives/ (December 2011)
The challenge of rational medicine’s journey from patient- to pathogen-specific
Recently, the New England Journal of Medicine (NEJM) released their 200th anniversary article titled, “Therapeutic Evolution and the Challenge of Rational Medicine,” by Greene et al. [1]. This article gives us a walkthrough of how medicine has evolved in the past 200 years: specifically, from patient-centered in approximately the first century and a half, to pathogen-centered in the last fifty or so years. Traditionally, western doctors had an in-depth knowledge of herbs — and a wide range of (often bizarre) treatments, ranging from the application of the “Devil’s dung” plant to the practice of bloodletting, i.e. “breathing a vein,” to assist in the curing of a disease. While some of these treatments are arguably questionable, specifically the well-versed knowledge of traditional western doctors focused more on the human perspective, and, as a result, may have been a vital ingredient to the overall well-being of the patient. This component appears lost today — where our healers are efficaciously oriented toward targeting a specific pathogen, with very specific aims. This compartmentalization of focus (generating doctors with specific knowledge about specific subjects) leaves patients with any other possible ailments or concerns to hang in the dark. While the light of the brilliant doctor who shines in his specific field of focus may isolate and treat the primary cause of a disease, the flashlight he is shining with on the patient may just as well blind the patient to any other factors just as important that could improve general well-being. The flashlight will of course cast shadows of its own. As the article in NEJM subtly points out, there can be no medicine without both therapeutic enthusiasm and therapeutic skepticism, and skepticism has flourished in the rationale of science ever since the chilling specter emerged from medicines such as thalidomide, Diethylstilbestrol, Vioxx, and Avandia [ibid]. These drugs were developed for specific purposes, i.e. to prevent morning tiredness, to act as an antidiabetic, etc., and while the focus of developing these drugs may have been done through well intention, the outcomes clearly revealed something menacing lurking in the shadows.
“As the locus of disease has narrowed from the afflicted person to the molecular mechanism, and the target of magic bullets has followed suit, physicians have faced regular reminders of the limits of the reductionist approach.” [1]
As we have been endlessly discovering smaller and smaller particles; and smaller and smaller actions that lead to larger reactions, one might wonder if this approach is the best to solely focus on. What may be an additional approach more fitting for our new century? The Shanghai Center for Systems Biomedicine has released an interesting article titled, “Toward new drugs for the human and non-human cells in people,” by Zhao et al. [2]. This explores the realization that the human body is only sparsely comprised of actual “human” cells. There is in fact a multitude of lifeforms that live within us and work in synergy with our body. For example, our metabolism is aided by lifeforms such as veillonella, bifidobacteria, and lactobacilli. Zhao et al. explain that humans are “superorganisms” due to the fact that we are 10% human cells and 90% microbes (primarily in the intestines).
“‘Super'” in that sense means ‘above and beyond.’ Scientists thus are viewing people as vast ecosystems in which human, bacterial, fungal and other cells interact with each another.” [2]
Therefore, when microbes significantly affect our genetic actions and reactions through gene regulation; i.e. on and off switching, this directly affects our immune response — and thus affects how diseases or disorders manifest. Due to this complexity, scientists realize how the reductionist approach can certainly fail — as all individuals will have a different response to treatment. We are complex beings and thus require complex interventions, and that certainly does not mean we should delve further to find even smaller particles or specialize ourselves even more. We should, on the contrary, seek a more holistic approach. For example, our own nutrition, diets, medications, mental state and physical activity (or lack thereof) completely affect the manifestation of our microbe populations within our bodies — and thus completely affect which genes are expressed and which are not. There is nature just as much as there is nurture. The so called “functional metagenomics” proposed by Zhao et al. [2] for developing new medicines that affect our microbes (and I say “our” for simplicity, because these organisms work together with us) are showing promise through traditional Chinese medicine (TCM) — an archaic yet thriving art of medicine that continues to prosper and grow in popularity even among the general scientific community as time passes. In the case of gene-environment reactions, most chronic conditions are involved. Here, Zhao et al. claim the gut microbiome is vital and TCM is tailored to target both the host as well as the synergistic microbes — thus being a holistic medicine, as treatments are not specifically tailored such as the conventional drug approach, which targets in an isolated fashion typical receptors within the “druggable genome.”
It appears that for the next age — moving on from an efficacious, isolated approach in primary care — we are not going back to a patient-centered approach which began in traditional western rational science, but rather a “super organismic” track that attempts to integrate as many human and non-human factors as possible.
References
1. Jeremy A. Greene, M.D., Ph.D., David S. Jones, M.D., Ph.D., and Scott H. Podolsky. M.D. Therapeutic Evolution and the Challenge of Rational Medicine. N Engl J Med 2012; 367:1077-1082. September 20, 2012. DOI: 10.1056/NEJMp1113570
2. Zhao L, Nicholson JK, Lu A, Wang Z, Tang H, Holmes E, Shen J, Zhang X, Li JV, Lindon JC. Targeting the human genome-microbiome axis for drug discovery: inspirations from global systems biology and traditional Chinese medicine. J Proteome Res. 2012 Jul 6;11(7):3509-19. Epub 2012 Jun 5.
23 and 1/2 hours

There seems to be one single, simple best thing to keep our lives healthy and to prevent especially non-communicable diseases: a small, but regular dose of physical activity. This is especially relevant for elderly people as they often suffer from multi-morbidity, but could potentially stay more healthy by changing their lifestyles just a little bit.
Wouldn’t it be easy to put eating and sleeping in 23 and 1/2 hours and keep 30 minutes for physical activit? It doesn’t even have to be on a daily basis, but e.g. going for a 30 minutes walk three times a week has already proven to reduce the risk for arthritis by 47%, for dementia by 50% and for diabetes by 58%.
So how about prescribing physical activity? If doctors did that for their patients – do you think it would have an impact on people’s health?
Check out this video by Michael Evans and Mercury Films Inc. http://www.youtube.com/watch?v=aUaInS6HIGo. It has also been posted by the Swedish Professional Association for Physical Activity. http://www.yfa.se/
Also check out Michael Evans’ blog: http://www.myfavouritemedicine.com/23-and-a-half-hours/
Council of Labor Affairs in Taiwan is Piloting A Programme That Will Provide The Elderly Accessibility To Foreign Caregivers on An Hourly Basis
Taiwan, like other places in Asia, is experiencing rapid ageing. According to some estimates, by 2025, the population of those over 65 years-of-age will be 20 percent, up from 8 percent in 2008. With a population just over 25 million, this represents a huge increase in a relatively short period of time–a problem further exacerbated with population trends such as increased women in the work-place, increased people living alone –being separated from the elderly, and decreased fertility.
Adequate manpower continues to represent a challenge, in part due to Taiwan’s strict laws on foreign immigration and caregiving but also due to the aforementioned trends, such as low fertility rates. Taiwan typically provides good care to veterans and old people, but little community support is available. Little government support is also provided to those who wish to age at home.
Despite this, most elderly Taiwanese prefer to age at home and, many of them, prefer to stay at home rather than go out and partake in community services. Given this fact, recently, Taiwan is undertaking a series of building projects aimed at building age-friendly environment to keep elderly energetic and age successfully at home.
However the issue still remains–with informal caregiving structures on the decline from more women participating in the work force and more elderly ageing at home, who will be able to care for the elderly as they choose to age at home?
Starting 2013, the Council of Labor Affairs will test out a pilot programme that will allow foreign workers to work part-time by the hour.
Citizens over the age of 80 who score 60 or less on the Bartel Index will be eligible to apply for part-time foreign caregiving services. Currently, due to immigration laws, only the elderly who suffer from 1-10 severe mental or physical disabilities and score lower than 35 on the Bartel Index/require around-the-clock care are eligible to employ a foreign caregiver.
Typically these caregivers are hired full-time and the employer is responsible for providing food and accommodation. With the new pilot, the arrangement will be quite different: rather than making employers responsible for housing and accommodation, part-time foreign workers will be employed by NGOs who will take responsibility for their well-being and care.
While there will be no limits on how many hours foreign caregivers can be hired for, their employment needs to be in-line with Taiwan’s Labor Standards Act. All agreements between caregivers and non-profit organisations are to be covered in a contract, stipulating what is expected on the part of both the employee and the employer.
Reimbursement issues are still to be defined at a later time between two parties: local governments and the non-profit organisations (the prospective employers).
Receiving full-time local home-based caregiving care, is available for those elderly at a much higher income bracket. However, there are also government-supported long-term care services available to the elderly, particularly for the veterans, the poor, and those with disabilities. If the elderly is a veteran, the veteran affairs commission provides homes and long-term care services. The Council for Agriculture provides some assistance for aged farmers. For poor elderly with mild-disabilities, the Ministry of Interior provides long-term care support such as step-down care facilities, home services, dementia day care and care in a community setting, and the Bureau of Nursing and Health provides long-term care services, such as nursing home care and home nursing/home care rehabilitation to the poor and disabled.
The new pilot programme then has the potential to cater to a new market of elderly–to allow elderly who are slightly more affluent but still low to middle, middle class, who may not be in need of full-time caregiving support and who wish to age at home–the ability to receive long-term care services from a foreign caregiver who may not be as costly as a local one and only for when needed. It still remains to be seen how this programme will be operationalised and will ensure that local caregivers are adequately provided for. Also, whether or not foreign caregivers will accept the contractual terms and be willing to be part-time caregivers in Taiwan.
Source: http://focustaiwan.tw/ShowNews/WebNews_Detail.aspx?Type=aSOC&ID=201209090012
U-health in Korea
Our teacher once accused us: “You’re incredible! What you guys don’t find on Wikipedia does not exist in your world – or what?”
Trying to find out more about “u-health”, I remembered that and it made me smile. U-health or u-health care cannot be found on Wikipedia (yet) and on the first sight it does not seem to be on many peoples’ minds in today’s world, but dig a little deeper!
U-health stands for ubiquitous health – omnipresent, universal, ever-present health. Sounds big! And there you go with your online-search… [Small note: I found so many interesting aspects that I don’t know where to start now – so let me just give you a basic idea with this blog post and let’s explore the topic further within the following ones.]
On the Congress on Nursing Informatics 2006 in Korea, u-health did cause lively discussions. The Korean Government had started a project on u-health services for the provision of health care services in the country’s rural areas using the advanced broadband infrastructure (NI 2006).
U-health care is a developing area of technology to monitor and improve a patient’s health status. It uses different environmental and patient sensors to gather data on almost any physiological characteristic to diagnose health problems (Brown et al. 2007). U-health should stand out through availability, transparency, seamlessness, awareness and trustworthiness – anytime and anywhere (Cha 2008).
Many industrialized countries are sitting on a demographic time bomb – facing problems in health care that are related to the growing number of elderly. Their limited resources in health need to be used more efficiently and effectively. So especially these societies could benefit from u-health care and its innovations to reach better diagnosis and treatment. It also has a lot of potential in improving hospital administration and patient management with reduction of medical errors, and in enhancing service quality, communication and collaboration. (Chang) However, at the same time, u-health care confronts ethical issues, e.g. when it comes to trust, privacy and liability, or in combining computer and information ethics with medical ethics (Brown 2007).
Hence, the bottom line is that yes, u-health is and will increasingly be on peoples’ minds (and it will probably soon appear on Wikipedia).
Societies as well as individuals will have to make difficult choices in the future.
1 Korea IT Times offers a variety of more interesting articles by Cha Joo-hak on the topic: http://www.koreaittimes.com/source/cha-joo-hak
2 Brown I and Adams A A 2007. The ethical challenges of ubiquitous healthcare. International Review of Information Ethics Vol. 8. www.i-r-i-e.net/inhalt/008/008_9.pdf
3 Cha J-H (2008). Defining the Perfect Ubiquitous Healthcare Information System. Korea IT Times. http://www.koreaittimes.com/story/56/defining-perfect-ubiquitous-healthcare-information-system
4 Cha J-H (2010)Who Shall Live Better? – Health Care and Socioeconomic Choice. Korea IT Times. http://www.koreaittimes.com/story/8559/who-shall-live-better-health-care-and-socioeconomic-choice
5 Chang B-C ().Ubiquitous-Healthcare Changed paradigm after introduction of EHR. Yonsei University. www.health-informatics.kk.usm.my/resources/2_Chang.pdf
6 NI 2006. The 9th International Congress on Nursing Informatics. Seoul, Korea June 2006. http://differance-engine.net/ni2006blog/?p=22